Acute appendicitis
Updates to Article Attributes
Acute appendicitis (plural: appendicitides) is an acute inflammation of the vermiform appendix. It is a very common condition in general radiology practice and is one of the main reasons for abdominal surgery in young patients. CT is the most sensitive modality to detect appendicitis.
Terminology
Appendicitis may be acute or chronic. Chronic appendicitis is an uncommon entity 25. Acute appendicitis may be simple/uncomplicated or complicated, depending on whether the patient has developed significant sequelae, i.e. by gangrene, abscess, or perforation.
If status post appendicectomy, then stump appendicitis may still occur.
If the appendix failed to descend normally during development then a subhepatic appendicitis may be seen.
Epidemiology
Acute appendicitis is typically a disease of children and young adults with a peak incidence in the 2nd to 3rd decades of life 1.
Clinical presentation
The classical presentation consists of periumbilical pain (referred) which within a day or later localises to the McBurney point with associated fever, nausea, and vomiting 2. This progression is only seen in a minority of cases and is unhelpful in children who often present with vague and non-specific signs and symptoms. It also relies on the appendix being in a 'normal' position, which is not the case in a significant number of cases (see below).
General signs and symptoms include 1,2:
-
localised pain and tenderness
right lower quadrant tenderness over appendix (i.e. McBurney sign)
pelvic pain, diarrhoea, and tenesmus (pelvic appendix)
flank pain (retrocaecal appendix)
groin pain - appendix within an inguinal hernia (Amyand hernia) or a femoral hernia (De Garengeot hernia)
right upper quadrant pain (subhepatic appendicitis) 22
leucocytosis
nausea and vomiting
-
atypical location:
within the pelvis (30%)
extraperitoneal (5%)
left iliac fossa (rare), found in patients with a long appendix, intestinal malrotation, situs inversus and those with a mobile caecum
Several clinical prediction and decision scores (rules) have been developed to improve diagnostic accuracy and reduce the rate of negative appendicectomies, some of which are in routine clinical use:
in children, clinicians sometimes use other scores such as a PAS or pARC score 3 for the same purpose
Pathology
Appendicitis is typically caused by obstruction of the appendiceal lumen, with the resultant build-up of fluid, suppurative inflammation, secondary infection, venous congestion, ischaemia and necrosis. Obstruction may be caused by 1,23:
lymphoid hyperplasia (~60%)
appendicolith (~33%)
foreign bodies (~4%)
Crohn disease or other rare causes, e.g. stricture, tumour, parasite
Radiographic features
One of the biggest challenges of imaging the appendix is finding it. Once confidently identified, assessing its normality is relatively straightforward.
Faecal loading of the caecum is associated with acute appendicitis, which is uncommon in other acute inflammatory diseases of the right side of the abdomen 24.
The location of the base of the appendix is relatively constant, located roughly between the ileocaecal valve and the apex of the caecum. This relationship is maintained even when the caecum is mobile.
The location of the tip of the appendix is much more variable, especially as the length of the appendix has an extensive range (2-20 cm) 9. The distribution of positions is described as 8,9:
behind the caecum (ascending retrocaecal): 65%
inferior to the caecum (subcaecal): 31%
behind the caecum (transverse retrocaecal): 2%
anterior to the ileum (ascending paracaecal preileal): 1%
posterior to the ileum (ascending paracaecal retroileal): 0.5%
Appendiceal diameter >6 mm has been commonly used as a cut-off for acute appendicitis but this has been shown as a sensitive but not specific sign of acute appendicits. The normal range of appendiceal diameter has been shown to be 2-13 mm (adults) 27 and 3-9 mm (paediastric) 28.
Plain radiograph
Plain radiography is infrequently able to give the diagnosis, however, is useful for identifying free gas, and may show an appendicolith in 7-15% of cases 1. In the right clinical setting, finding an appendicolith makes the probability of acute appendicitis up to 90%.
If an inflammatory phlegmon is present, displacement of caecal gas with mural thickening may be evident.
Small bowel obstruction pattern with small bowel dilatation and air-fluid levels is present in ~40% of perforations.
Ultrasound
Ultrasound with its lack of ionising radiation should be the investigation of choice in young patients. With a competent user, ultrasonography is reliable at identifying abnormal appendices, especially in thin patients. However, the identification of a normal appendix is more problematic, and in many instances, appendicitis cannot be ruled out.
The technique used is known as graded compression, using the linear probe over the site of maximal tenderness, with gradual increasing pressure exerted to displace normal overlying bowel gas.
Findings supportive of the diagnosis of appendicitis include 5:
-
aperistaltic, non-compressible, dilated appendix (>6 mm outer diameter)
appears round when compression is applied
hyperechoic appendicolith with posterior acoustic shadowing
-
distinct appendiceal wall layers
implies non-necrotic (catarrhal or phlegmon) stage
loss of wall stratification with necrotic (gangrenous) stages 18
echogenic prominent pericaecal and periappendiceal fat
periappendiceal hyperechoic structure: amorphous hyperechoic structure (usually >10 mm) seen surrounding a non-compressible appendix with a diameter >6 mm 11
periappendiceal fluid collection
target appearance (axial section)
periappendiceal reactive nodal prominence/enlargement
-
wall thickening (3 mm or above)
mural hyperaemia with colour flow Doppler increases the specificity 17
vascular flow may be lost with necrotic stages
-
alteration of the mural spectral Doppler envelope 16
may support diagnosis in equivocal cases
a peak systolic velocity >10 cm/s suggested as a cutoff
a resistive index (RI) measured at >0.65 may be more specific
Confirming that the structure visualised in the appendix is clearly essential and requires demonstration of it being blind-ending and arising from the base of the caecum. Identifying the terminal ileum confidently is also helpful.
A dynamic ultrasound technique using a sequential 3-step patient positioning protocol has been shown to increase the detection rate of appendix 10. In the study, patients were initially examined in the conventional supine position, followed by the left posterior oblique position (45° LPO) and then a “second-look” supine position. Reported detection rates increased from 30% in the initial supine position to 44% in the LPO position and a further increase to 53% with the “second-look” supine position. Slightly larger absolute and relative detection rates were seen in children. The authors suggested that the effect of the LPO positioning step improved the acoustic window by shifting bowel contents.
CT
CT is highly sensitive (94-98%) and specific (up to 97%) for the diagnosis of acute appendicitis and allows for alternative causes of abdominal pain also to be diagnosed. The need for contrast (IV, oral or both) is debatable and varies from institution to institution. Oral contrast has not been shown to increase the sensitivity of CT 12. Nonetheless, many radiologists advocate the use of oral contrast in patients with a low BMI (<25).
CT findings include 1,2,4:
appendiceal dilatation (>6 mm outer diameter) 4
wall thickening (>3 mm) and enhancement
thickening of the caecal apex: caecal bar sign, arrowhead sign
intraluminal fluid depth >2.6 mm in a dilated (>6 mm) appendix without periappendiceal inflammation 29
-
periappendiceal inflammation
fat stranding
thickening of the lateroconal fascia or mesoappendix
extraluminal fluid
phlegmon (inflammatory mass)
abscess
focal wall non-enhancement representing necrosis (gangrenous appendicitis) and a precursor to perforation
Less specific signs may be associated with appendicitis:
periappendiceal reactive nodal enlargement
{{youtube:https://www.youtube.com/watch?v=BI6BgaX6u2k}}
MRI
MRI is recommended as the second-line modality for suspected acute appendicitis in pregnancypregnant patients, where available 14,15. Protocols vary widely, but most include imaging in three planes with a rapidly acquired sequence with T2 weighting, and some include T2 fat-suppressed imaging. MRI findings mirror those of other modalities, with luminal distension and widening, wall thickening, and periappendiceal free fluid.
Treatment and prognosis
Treatment is appendicectomy, which can be performed either open or laparoscopically 6. Mortality from simple appendicitis is approximately 0.1% but is as high as 5% in perforation with generalised peritonitis 6.
In ~30% of cases where the appendix has become gangrenous and perforated, initial nonoperative management is preferred provided the patient is stable. It is inIn this situation that, radiologists have a therapeutic role to play with percutaneous CT- or US-guided drainages of periappendiceal abscess.
Complications
Recognised complications include 6:
-
perforation: in 10-20% of cases 21
most specifically suggested by appendiceal abscess or extraluminal gas, but commonly also seen as periappendiceal phlegmon and fluid 20
generalised peritonitis due to free perforation
pylephlebitis: infective thrombophlebitis of the portal circulation
When a complication occurs, it is said to be "complicated appendicitis".
Differential diagnosis
Clinically, the most common differential is that of mesenteric adenitis, which can be differentiated by the identification of a normal appendix and enlarged mesenteric lymph nodes.
The imaging differential includes:
inflammatory bowel disease, especially Crohn disease, which may affect the appendix
other causes of terminal ileitis
lymphoid hyperplasia
right-sided diverticulitis
acute epiploic appendagitis
isolated appendiceal submucosal lipomatosis 26
Valentino syndrome (from perforated peptic ulcer)
enlarged normal appendix as almost 50% of asymptomatic patients can have an appendix diameter greater than 6 mm on CT 13
Practical points
on CT, identify first the ileocaecal valve, which usually has fatty lips, and then look for the appendix more inferiorly on the same side
>6 mm outer diameter is a reliable measurement to characterise appendicitis in all imaging modalities
inflammation may be initially limited to the distal end of the appendix (tip appendicitis). It is crucial (particularly with US) to completely evaluate the appendix, and consider further assessment with cross-sectional imaging if it is only partially visualised, but the patient is clinically suspicious
prior appendicectomy does not completely rule out a recurrent stump appendicitis, the risk of which is significant if the appendiceal remnant is greater than 5 mm
appendiceal endometriosis is not uncommon, affecting 4-22% of patients with endometriosis, and is a challenging diagnosis on imaging. Nodular, inhomogeneous appendiceal thickening combined with non-specific, often cyclical symptoms can be hints of this condition 23
See also
-<p><strong>Acute appendicitis</strong> (plural: appendicitides) is an acute inflammation of the <a href="/articles/appendix-1">vermiform appendix</a>. It is a very common condition in general radiology practice and is one of the main reasons for abdominal surgery in young patients. CT is the most sensitive modality to detect appendicitis.</p><h4>Terminology</h4><p>Appendicitis may be acute or chronic. <a href="/articles/chronic-appendicitis">Chronic appendicitis</a> is an uncommon entity <sup>25</sup>. Acute appendicitis may be simple/uncomplicated or complicated, depending on whether the patient has developed significant sequelae, i.e. <a href="/articles/gangrenous-appendix">gangrene</a>, <a href="/articles/appendicular-abscess">abscess</a>, <a href="/articles/perforated-appendix">perforation</a>. </p><p>If <a href="/articles/status-post">status post</a> appendicectomy, then <a href="/articles/stump-appendicitis">stump appendicitis</a> may still occur.</p><p>If the appendix failed to descend normally during development then a <a href="/articles/subhepatic-appendicitis">subhepatic appendicitis</a> may be seen.</p><h4>Epidemiology</h4><p>Acute appendicitis is typically a disease of children and young adults with a peak incidence in the 2<sup>nd </sup>to 3<sup>rd</sup> decades of life <sup>1</sup>.</p><h4>Clinical presentation</h4><p>The classical presentation consists of periumbilical pain (referred) which within a day or later localises to <a href="/articles/mcburney-point">McBurney point</a> with associated fever, nausea, and vomiting <sup>2</sup>. This progression is only seen in a minority of cases and is unhelpful in children who often present with vague and non-specific signs and symptoms. It also relies on the appendix being in a 'normal' position, which is not the case in a significant number of cases (see below).</p><p>General signs and symptoms include <sup>1,2</sup>:</p><ul>- +<p><strong>Acute appendicitis</strong> (plural: appendicitides) is an acute inflammation of the <a href="/articles/appendix-1">vermiform appendix</a>. It is a very common condition in general radiology practice and is one of the main reasons for abdominal surgery in young patients. CT is the most sensitive modality to detect appendicitis.</p><h4>Terminology</h4><p>Appendicitis may be acute or chronic. <a href="/articles/chronic-appendicitis">Chronic appendicitis</a> is an uncommon entity <sup>25</sup>. Acute appendicitis may be simple/uncomplicated or complicated by <a href="/articles/gangrenous-appendix">gangrene</a>, <a href="/articles/appendicular-abscess">abscess</a>, or <a href="/articles/perforated-appendix">perforation</a>. </p><p>If <a href="/articles/status-post">status post</a> appendicectomy, then <a href="/articles/stump-appendicitis">stump appendicitis</a> may still occur.</p><p>If the appendix failed to descend normally during development then a <a href="/articles/subhepatic-appendicitis">subhepatic appendicitis</a> may be seen.</p><h4>Epidemiology</h4><p>Acute appendicitis is typically a disease of children and young adults with a peak incidence in the 2<sup>nd </sup>to 3<sup>rd</sup> decades of life <sup>1</sup>.</p><h4>Clinical presentation</h4><p>The classical presentation consists of periumbilical pain (referred) which within a day or later localises to the <a href="/articles/mcburney-point">McBurney point</a> with associated fever, nausea, and vomiting <sup>2</sup>. This progression is only seen in a minority of cases and is unhelpful in children who often present with vague and non-specific signs and symptoms. It also relies on the appendix being in a 'normal' position, which is not the case in a significant number of cases (see below).</p><p>General signs and symptoms include <sup>1,2</sup>:</p><ul>
-</ul><p>{{youtube:https://www.youtube.com/watch?v=BI6BgaX6u2k}}</p><h5>MRI</h5><p>MRI is recommended as the second-line modality for suspected acute appendicitis in pregnancy patients, where available <sup>14,15</sup>. Protocols vary widely, but most include imaging in three planes with a rapidly acquired sequence with T2 weighting, and some include T2 fat-suppressed imaging. MRI findings mirror those of other modalities, with luminal distension and widening, wall thickening, and periappendiceal free fluid.</p><h4>Treatment and prognosis</h4><p>Treatment is <a href="/articles/appendectomy">appendicectomy</a>, which can be performed either open or laparoscopically <sup>6</sup>. Mortality from simple appendicitis is approximately 0.1% but is as high as 5% in perforation with generalised peritonitis <sup>6</sup>.</p><p>In ~30% of cases where the appendix has become gangrenous and perforated, initial nonoperative management is preferred provided the patient is stable. It is in this situation that radiologists have a therapeutic role to play with percutaneous CT- or US-guided drainages of periappendiceal abscess.</p><h5>Complications</h5><p>Recognised complications include <sup>6</sup>:</p><ul>- +</ul><p>{{youtube:https://www.youtube.com/watch?v=BI6BgaX6u2k}}</p><h5>MRI</h5><p>MRI is recommended as the second-line modality for suspected acute appendicitis in pregnant patients, where available <sup>14,15</sup>. <a href="/articles/abdominal-pain-in-pregnancy-protocol-mri" title="Abdominal pain in pregnancy protocol (MRI)">Protocols</a> vary widely, but most include imaging in three planes with a rapidly acquired sequence with T2 weighting, and some include T2 fat-suppressed imaging. MRI findings mirror those of other modalities, with luminal distension and widening, wall thickening, and periappendiceal free fluid.</p><h4>Treatment and prognosis</h4><p>Treatment is <a href="/articles/appendectomy">appendicectomy</a>, which can be performed either open or laparoscopically <sup>6</sup>. Mortality from simple appendicitis is approximately 0.1% but is as high as 5% in perforation with generalised peritonitis <sup>6</sup>.</p><p>In ~30% of cases where the appendix has become gangrenous and perforated, initial nonoperative management is preferred provided the patient is stable. In this situation, radiologists have a therapeutic role to play with percutaneous CT- or US-guided drainages of periappendiceal abscess.</p><h5>Complications</h5><p>Recognised complications include <sup>6</sup>:</p><ul>
References changed:
- 1. Weissleder R. Primer of Diagnostic Imaging. (2007) ISBN: 9780323040686 - <a href="http://books.google.com/books?vid=ISBN9780323040686">Google Books</a>
- 2. Callahan M, Rodriguez D, Taylor G. CT of Appendicitis in Children. Radiology. 2002;224(2):325-32. <a href="https://doi.org/10.1148/radiol.2242010998">doi:10.1148/radiol.2242010998</a> - <a href="https://www.ncbi.nlm.nih.gov/pubmed/12147823">Pubmed</a>
- 3. Cotton D, Vinson D, Vazquez-Benitez G et al. Validation of the Pediatric Appendicitis Risk Calculator (PARC) in a Community Emergency Department Setting. Ann Emerg Med. 2019;74(4):471-80. <a href="https://doi.org/10.1016/j.annemergmed.2019.04.023">doi:10.1016/j.annemergmed.2019.04.023</a> - <a href="https://www.ncbi.nlm.nih.gov/pubmed/31229394">Pubmed</a>
- 4. Pereira J, Sirlin C, Pinto P, Jeffrey R, Stella D, Casola G. Disproportionate Fat Stranding: A Helpful CT Sign in Patients with Acute Abdominal Pain. Radiographics. 2004;24(3):703-15. <a href="https://doi.org/10.1148/rg.243035084">doi:10.1148/rg.243035084</a> - <a href="https://www.ncbi.nlm.nih.gov/pubmed/15143223">Pubmed</a>
- 5. Puylaert J. Acute Appendicitis: US Evaluation Using Graded Compression. Radiology. 1986;158(2):355-60. <a href="https://doi.org/10.1148/radiology.158.2.2934762">doi:10.1148/radiology.158.2.2934762</a> - <a href="https://www.ncbi.nlm.nih.gov/pubmed/2934762">Pubmed</a>
- 6. Doherty GM, Way LW. Current Surgical Diagnosis & Treatment. (2006) ISBN: 007142315X - <a href="http://books.google.com/books?vid=ISBN007142315X">Google Books</a>
- 11. Noguchi T, Yoshimitsu K, Yoshida M. Periappendiceal Hyperechoic Structure on Sonography: A Sign of Severe Appendicitis. J Ultrasound Med. 2005;24(3):323-7; quiz 328. <a href="https://doi.org/10.7863/jum.2005.24.3.323">doi:10.7863/jum.2005.24.3.323</a> - <a href="https://www.ncbi.nlm.nih.gov/pubmed/15723844">Pubmed</a>
- 16. Shin L, Jeffrey R, Berry G, Olcott E. Spectral Doppler Waveforms for Diagnosis of Appendicitis: Potential Utility of Point Peak Systolic Velocity and Resistive Index Values. Radiology. 2017;285(3):990-8. <a href="https://doi.org/10.1148/radiol.2017162251">doi:10.1148/radiol.2017162251</a> - <a href="https://www.ncbi.nlm.nih.gov/pubmed/28582634">Pubmed</a>
- 18. James A. Connolly, Anthony J. Dean, Beatrice Hoffmann et al. Emergency Point-Of-Care Ultrasound. (2017) ISBN: 9780470657577 - <a href="http://books.google.com/books?vid=ISBN9780470657577">Google Books</a>
- 19. Lim H, Lee W, Kim T, Namgung S, Lee S, Lim J. Appendicitis: Usefulness of Color Doppler US. Radiology. 1996;201(1):221-5. <a href="https://doi.org/10.1148/radiology.201.1.8816547">doi:10.1148/radiology.201.1.8816547</a> - <a href="https://www.ncbi.nlm.nih.gov/pubmed/8816547">Pubmed</a>
- 20. Avanesov M, Wiese N, Karul M et al. Diagnostic Prediction of Complicated Appendicitis by Combined Clinical and Radiological Appendicitis Severity Index (APSI). Eur Radiol. 2018;28(9):3601-10. <a href="https://doi.org/10.1007/s00330-018-5339-9">doi:10.1007/s00330-018-5339-9</a> - <a href="https://www.ncbi.nlm.nih.gov/pubmed/29541911">Pubmed</a>
- 22. Ball W & Privitera A. Subhepatic Appendicitis: A Diagnostic Dilemma. BMJ Case Rep. 2013;2013(apr18 1):bcr2013009454. <a href="https://doi.org/10.1136/bcr-2013-009454">doi:10.1136/bcr-2013-009454</a> - <a href="https://www.ncbi.nlm.nih.gov/pubmed/23605843">Pubmed</a>
- 25. Checkoff J, Wechsler R, Nazarian L. Chronic Inflammatory Appendiceal Conditions That Mimic Acute Appendicitis on Helical CT. AJR Am J Roentgenol. 2002;179(3):731-4. <a href="https://doi.org/10.2214/ajr.179.3.1790731">doi:10.2214/ajr.179.3.1790731</a> - <a href="https://www.ncbi.nlm.nih.gov/pubmed/12185054">Pubmed</a>
- 27. Rettenbacher T, Hollerweger A, Macheiner P et al. Outer Diameter of the Vermiform Appendix as a Sign of Acute Appendicitis: Evaluation at US. Radiology. 2001;218(3):757-62. <a href="https://doi.org/10.1148/radiology.218.3.r01fe20757">doi:10.1148/radiology.218.3.r01fe20757</a> - <a href="https://www.ncbi.nlm.nih.gov/pubmed/11230651">Pubmed</a>
- 28. Trout A, Towbin A, Zhang B. Journal Club: The Pediatric Appendix: Defining Normal. AJR Am J Roentgenol. 2014;202(5):936-45. <a href="https://doi.org/10.2214/AJR.13.11030">doi:10.2214/AJR.13.11030</a> - <a href="https://www.ncbi.nlm.nih.gov/pubmed/24758645">Pubmed</a>
- 29. Moteki T & Horikoshi H. New CT Criterion for Acute Appendicitis: Maximum Depth of Intraluminal Appendiceal Fluid. AJR Am J Roentgenol. 2007;188(5):1313-9. <a href="https://doi.org/10.2214/AJR.06.1180">doi:10.2214/AJR.06.1180</a> - <a href="https://www.ncbi.nlm.nih.gov/pubmed/17449776">Pubmed</a>
- 1. Ralph Weissleder. Primer of Diagnostic Imaging with CD-ROM. (2006) ISBN: 0323040683
- 2. Callahan M, Rodriguez D, Taylor G. CT of Appendicitis in Children. Radiology. 2002;224(2):325-32. <a href="https://doi.org/10.1148/radiol.2242010998">doi:10.1148/radiol.2242010998</a>
- 3. Cotton D, Vinson D, Vazquez-Benitez G et al. Validation of the Pediatric Appendicitis Risk Calculator (PARC) in a Community Emergency Department Setting. Ann Emerg Med. 2019;74(4):471-80. <a href="https://doi.org/10.1016/j.annemergmed.2019.04.023">doi:10.1016/j.annemergmed.2019.04.023</a>
- 4. Pereira J, Sirlin C, Pinto P, Jeffrey R, Stella D, Casola G. Disproportionate Fat Stranding: A Helpful CT Sign in Patients with Acute Abdominal Pain. Radiographics. 2004;24(3):703-15. <a href="https://doi.org/10.1148/rg.243035084">doi:10.1148/rg.243035084</a>
- 5. Puylaert J. Acute Appendicitis: US Evaluation Using Graded Compression. Radiology. 1986;158(2):355-60. <a href="https://doi.org/10.1148/radiology.158.2.2934762">doi:10.1148/radiology.158.2.2934762</a>
- 6. Gerard M. Doherty, Lawrence W. Way. Current Surgical Diagnosis & Treatment (Current Surgical Diagnosis and Treatment). (2005) ISBN: 007142315X
- 11. Noguchi T, Yoshimitsu K, Yoshida M. Periappendiceal Hyperechoic Structure on Sonography. J Ultrasound Med. 2005;24(3):323-7. <a href="https://doi.org/10.7863/jum.2005.24.3.323">doi:10.7863/jum.2005.24.3.323</a> - <a href="https://www.ncbi.nlm.nih.gov/pubmed/15723844">Pubmed</a>
- 16. Shin L, Jeffrey R, Berry G, Olcott E. Spectral Doppler Waveforms for Diagnosis of Appendicitis: Potential Utility of Point Peak Systolic Velocity and Resistive Index Values. Radiology. 2017;285(3):990-8. <a href="https://doi.org/10.1148/radiol.2017162251">doi:10.1148/radiol.2017162251</a>
- 18. Bob Jarman. Emergency Point-Of-Care Ultrasound. (2017) ISBN: 9780470657577
- 19. Lim H, Lee W, Kim T, Namgung S, Lee S, Lim J. Appendicitis: Usefulness of Color Doppler US. Radiology. 1996;201(1):221-5. <a href="https://doi.org/10.1148/radiology.201.1.8816547">doi:10.1148/radiology.201.1.8816547</a>
- 20. Avanesov M, Wiese N, Karul M et al. Diagnostic Prediction of Complicated Appendicitis by Combined Clinical and Radiological Appendicitis Severity Index (APSI). Eur Radiol. 2018;28(9):3601-10. <a href="https://doi.org/10.1007/s00330-018-5339-9">doi:10.1007/s00330-018-5339-9</a>
- 22. Ball W & Privitera A. Subhepatic Appendicitis: A Diagnostic Dilemma. Case Reports. 2013;2013(apr18 1):bcr2013009454. <a href="https://doi.org/10.1136/bcr-2013-009454">doi:10.1136/bcr-2013-009454</a> - <a href="https://www.ncbi.nlm.nih.gov/pubmed/23605843">Pubmed</a>
- 25. Checkoff J, Wechsler R, Nazarian L. Chronic Inflammatory Appendiceal Conditions That Mimic Acute Appendicitis on Helical CT. AJR Am J Roentgenol. 2002;179(3):731-4. <a href="https://doi.org/10.2214/ajr.179.3.1790731">doi:10.2214/ajr.179.3.1790731</a>
- 27. Rettenbacher T, Hollerweger A, Macheiner P et al. Outer Diameter of the Vermiform Appendix as a Sign of Acute Appendicitis: Evaluation at US. Radiology. 2001;218(3):757-62. <a href="https://doi.org/10.1148/radiology.218.3.r01fe20757">doi:10.1148/radiology.218.3.r01fe20757</a>
- 28. Trout A, Towbin A, Zhang B. JOURNAL CLUB: The Pediatric Appendix: Defining Normal. AJR Am J Roentgenol. 2014;202(5):936-45. <a href="https://doi.org/10.2214/ajr.13.11030">doi:10.2214/ajr.13.11030</a> - <a href="https://www.ncbi.nlm.nih.gov/pubmed/24758645">Pubmed</a>
- 29. Moteki T & Horikoshi H. New CT Criterion for Acute Appendicitis: Maximum Depth of Intraluminal Appendiceal Fluid. AJR Am J Roentgenol. 2007;188(5):1313-9. <a href="https://doi.org/10.2214/ajr.06.1180">doi:10.2214/ajr.06.1180</a> - <a href="https://www.ncbi.nlm.nih.gov/pubmed/17449776">Pubmed</a>
Image ( destroy )
Image ( destroy )
Image ( destroy )
Image ( destroy )
Image ( destroy )
Image ( destroy )
Image ( destroy )
Image ( destroy )
Image ( destroy )
Image ( destroy )
Image ( destroy )
Image ( destroy )
Image ( destroy )
Image ( destroy )
Image ( destroy )
Image ( destroy )
Image ( destroy )
Image ( update )
Image ( update )
Image ( update )
Image 2 Photo ( update )

Image 3 Pathology (Gross pathology) ( update )

Image 5 Ultrasound (Transverse) ( update )

Image 6 Ultrasound ( update )

Image 7 Ultrasound ( update )

Image 8 Ultrasound ( update )

Image 9 Ultrasound ( update )

Image 10 Ultrasound ( update )

Image 12 CT (C+ portal venous phase) ( update )

Image 13 CT (C+ portal venous phase) ( update )

Image 14 CT (C+ portal venous phase) ( update )

Image 15 CT (C+ portal venous phase) ( update )

Image 16 CT (C+ portal venous phase) ( update )

Image 17 CT (C+ portal venous phase) ( update )

Image 18 CT (C+ portal venous phase) ( update )

Image 19 CT (C+ portal venous phase) ( update )

Image 20 MRI (Gradient Echo fat saturated) ( update )

Image 21 MRI (T2) ( update )
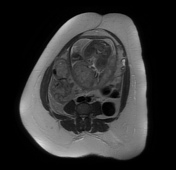
Image 22 MRI (T2) ( update )

Image 23 MRI (DWI) ( update )







 Unable to process the form. Check for errors and try again.
Unable to process the form. Check for errors and try again.