Choledocholithiasis
Updates to Article Attributes
Choledocholithiasis denotes the presence of gallstones within the bile ducts (including the common hepatic duct/common bile duct).
Epidemiology
Choledocholithiasis is relatively common, seen in up to 20% of patients undergoing cholecystectomy for gallstone-related complaints 2.
Clinical presentation
Stones within the bile ducts are oftenoccasionally asymptomatic and may be found incidentally, however. However, more frequently they lead to symptomatic presentation with:
Pathology
Stones within the bile duct most commonly pass from the gallbladder but may form in situ. When recurrent, they tend to be pigment stones, and are thought to be associated with bacterial infection 1.
Radiographic features
Ultrasound
Although ultrasound is usually the first investigation for biliary disease, it has average sensitivity for the detection of biliary stones within the bile duct.
Ultrasound should be performed both longitudinally and transversely through the duct with particular attention paid to the very distal portion of the common bile duct as it passes through the pancreatic head (best assessed transversely).
Findings include:
-
visualisation of stone(s)
echogenic rounded focus
size ranges between 2 to >20 mm
shadowing may be more difficult to elicit than with gallstones within the gallbladder
~20% of common bile duct stones will not shadow
twinkling artifact may be useful to detect occult stones
-
dilated bile duct
>6 mm + 1 mm per decade above 60 years of age
>10 mm post-cholecystectomy
dilated intrahepatic biliary tree
gallstones should increase suspicion, especially if multiple and small
Recently endoscopic ultrasonography (EUS) has also been used with very high sensitivity and specificity.
CT
Routine contrast-enhanced CT is moderately sensitive to choledocholithiasis with a sensitivity of 65-88% 3, but it requires attention to a number of potentially subtle findings. These include:
-
central rounded density: stone
surrounding lower attenuating bile or mucosa
rim sign: stone is outlined by thin shell of density
crescent sign: bile eccentrically outlines luminal stone, creating a low attenuation crescent
calcification of the stone: unfortunately only 20% of stones are of high density
Setting window level to the mean of the bile duct and setting the window width to 150 HU has been reported to improve sensitivity.
Biliary dilatation may also be visible.
CT cholangiography
CT with prior administration of biliary excreted contrast agents is highly sensitive (88-96%) and specific (88-98%) 8 for choledocholithiasis. The difficulty is, however, two-fold:
contrast agents have relatively high complication rates
obstructive cholestasis diminishes excretion, and thus is only viable in patients with largely normal liver function tests
MRCP
Magnetic resonance cholangiopancreatography (MRCP) has largely replaced ERCP as the gold standard for diagnosis of choledocholithiasis, able to achieve similar sensitivity (90-94%) and specificity (95-99%) 7,8 without ionising radiation, intravenous contrast, or the complication rate inherent in ERCP.
Filling defects are seen within the biliary tree on thin cross-sectional T2 weighted imaging. Care should be taken not to use thick slabs for the diagnosis as volume averaging may obscure smaller stones.
However, if the diagnosis has already been secured by ultrasound or CT, there is no additional value of MRCP, and the next step is therapeutic ERCP (see below).
Percutaneous or oral cholangiography
Both investigations are no longer used for routine diagnosis having been replaced by ultrasound, CT and MRCP.
Treatment and prognosis
Endoscopic retrograde cholangiopancreatography (ERCP) with sphincterotomy is the treatment of choice for choledocholithiasis, however, is associated with a complication rate of 5.8-24% (10 years follow-up) 1.
Complications of ERCP and sphincterotomy include:
perforation of oesophagus, stomach or duodenum due to endoscopy
Failure of endoscopic clearance of bile duct stones may require either intraoperative bile duct exploration, or percutaneous biliary drainage to decompress the biliary system to temporise and allow subsequent definitive management.
Differential diagnosis
There is usually little differential, and differential will depend on the modality. The most frequent entities to consider include:
-
malignancies
ampulla of Vater carcinoma: arises from a distal position, at the pancreaticobiliary junction, and has low attenuation
-
other filling defects
air bubbles
parasites
-
mimics
partial volume averaging of bowel gas
vascular calcification
surgical clips
-
MRCP specific potential pitfalls 6
vascular impressions
sphincteric contraction or pseudocalculus sign
-<p><strong>Choledocholithiasis</strong> denotes the presence of <a href="/articles/gallstones-1">gallstones</a> within the <a href="/articles/bile-duct">bile ducts</a> (including the common hepatic duct/common bile duct).</p><h4>Epidemiology</h4><p>Choledocholithiasis is relatively common, seen in up to 20% of patients undergoing cholecystectomy for gallstone-related complaints <sup>2</sup>.</p><h4>Clinical presentation</h4><p>Stones within the bile ducts are often asymptomatic and may be found incidentally, however, more frequently they lead to symptomatic presentation with:</p><ul>-<li><a href="/articles/biliary-colic">biliary colic</a></li>-<li><a href="/articles/ascending-cholangitis">ascending cholangitis</a></li>-<li><a href="/articles/jaundice">obstructive jaundice</a></li>-<li><a href="/articles/acute-pancreatitis">acute pancreatitis</a></li>- +<p><strong>Choledocholithiasis</strong> denotes the presence of <a href="/articles/gallstones-1">gallstones</a> within the <a href="/articles/bile-duct">bile ducts</a> (including the common hepatic duct/common bile duct).</p><h4>Epidemiology</h4><p>Choledocholithiasis is relatively common, seen in up to 20% of patients undergoing cholecystectomy for gallstone-related complaints <sup>2</sup>.</p><h4>Clinical presentation</h4><p>Stones within the bile ducts are occasionally asymptomatic and may be found incidentally. However, more frequently they lead to symptomatic presentation with:</p><ul>
- +<li><p><a href="/articles/biliary-colic">biliary colic</a></p></li>
- +<li><p><a href="/articles/ascending-cholangitis">ascending cholangitis</a></p></li>
- +<li><p><a href="/articles/jaundice">obstructive jaundice</a></p></li>
- +<li><p><a href="/articles/acute-pancreatitis">acute pancreatitis</a></p></li>
-<li>visualisation of stone(s)<ul>-<li>echogenic rounded focus</li>-<li>size ranges between 2 to >20 mm</li>-<li>shadowing may be more difficult to elicit than with gallstones within the gallbladder</li>-<li>~20% of common bile duct stones will not shadow</li>-<a href="/articles/twinkling-artifact">twinkling artifact</a> may be useful to detect occult stones</li>- +<p>visualisation of stone(s)</p>
- +<ul>
- +<li><p>echogenic rounded focus</p></li>
- +<li><p>size ranges between 2 to >20 mm</p></li>
- +<li><p>shadowing may be more difficult to elicit than with gallstones within the gallbladder</p></li>
- +<li><p>~20% of common bile duct stones will not shadow</p></li>
- +<li><p><a href="/articles/twinkling-artifact">twinkling artifact</a> may be useful to detect occult stones</p></li>
-<li>dilated bile duct<ul>-<li>>6 mm + 1 mm per decade above 60 years of age</li>-<li>>10 mm post-cholecystectomy</li>-<li>dilated intrahepatic biliary tree</li>- +<li>
- +<p>dilated bile duct</p>
- +<ul>
- +<li><p>>6 mm + 1 mm per decade above 60 years of age</p></li>
- +<li><p>>10 mm post-cholecystectomy</p></li>
- +<li><p>dilated intrahepatic biliary tree</p></li>
-<li>gallstones should increase suspicion, especially if multiple and small</li>- +<li><p>gallstones should increase suspicion, especially if multiple and small</p></li>
-<a href="/articles/target-sign-choledocholithiasis">target sign</a><ul>-<li>central rounded density: stone</li>-<li>surrounding lower attenuating bile or mucosa</li>- +<p><a href="/articles/target-sign-choledocholithiasis">target sign</a></p>
- +<ul>
- +<li><p>central rounded density: stone</p></li>
- +<li><p>surrounding lower attenuating bile or mucosa</p></li>
-<li>-<a href="/articles/rim-sign-of-choledocholithiasis">rim sign</a>: stone is outlined by thin shell of density</li>-<li>-<a href="/articles/crescent-sign-of-arterial-dissection">crescent sign</a>: bile eccentrically outlines luminal stone, creating a low attenuation crescent</li>-<li>calcification of the stone: unfortunately only 20% of stones are of high density</li>- +<li><p><a href="/articles/rim-sign-of-choledocholithiasis">rim sign</a>: stone is outlined by thin shell of density</p></li>
- +<li><p><a href="/articles/crescent-sign-of-arterial-dissection">crescent sign</a>: bile eccentrically outlines luminal stone, creating a low attenuation crescent</p></li>
- +<li><p>calcification of the stone: unfortunately only 20% of stones are of high density</p></li>
-<li>contrast agents have relatively high complication rates</li>-<li>obstructive cholestasis diminishes excretion, and thus is only viable in patients with largely normal liver function tests</li>- +<li><p>contrast agents have relatively high complication rates</p></li>
- +<li><p>obstructive cholestasis diminishes excretion, and thus is only viable in patients with largely normal liver function tests</p></li>
-<li><a href="/articles/acute-pancreatitis">acute pancreatitis</a></li>-<li><a href="/articles/acute-cholangitis">acute cholangitis</a></li>-<li>-<a href="/articles/oesophageal-perforation">perforation of oesophagus</a>, stomach or duodenum due to endoscopy</li>- +<li><p><a href="/articles/acute-pancreatitis">acute pancreatitis</a></p></li>
- +<li><p><a href="/articles/acute-cholangitis">acute cholangitis</a></p></li>
- +<li><p><a href="/articles/oesophageal-perforation">perforation of oesophagus</a>, stomach or duodenum due to endoscopy</p></li>
-<li>malignancies<ul>-<li><a href="/articles/cholangiocarcinoma">cholangiocarcinoma</a></li>-<a href="/articles/ampulla-of-vater-carcinoma">ampulla of Vater carcinoma</a>: arises from a distal position, at the pancreaticobiliary junction, and has low attenuation</li>-<li><a href="/articles/pancreatic-ductal-adenocarcinoma-4">pancreatic adenocarcinoma</a></li>- +<p>malignancies</p>
- +<ul>
- +<li><p><a href="/articles/cholangiocarcinoma">cholangiocarcinoma</a></p></li>
- +<li><p><a href="/articles/ampulla-of-vater-carcinoma">ampulla of Vater carcinoma</a>: arises from a distal position, at the pancreaticobiliary junction, and has low attenuation</p></li>
- +<li><p><a href="/articles/pancreatic-ductal-adenocarcinoma-4">pancreatic adenocarcinoma</a></p></li>
-<li>other filling defects<ul>-<li>air bubbles</li>-<li>parasites</li>- +<li>
- +<p>other filling defects</p>
- +<ul>
- +<li><p>air bubbles</p></li>
- +<li><p>parasites</p></li>
-<li>mimics<ul>-<li>partial volume averaging of bowel gas</li>-<li>vascular calcification</li>-<li>surgical clips</li>- +<li>
- +<p>mimics</p>
- +<ul>
- +<li><p>partial volume averaging of bowel gas</p></li>
- +<li><p>vascular calcification</p></li>
- +<li><p>surgical clips</p></li>
-<li>MRCP specific potential pitfalls <sup>6</sup><ul>-<li><a href="/articles/magnetic-susceptibility-artifact">susceptibility artifacts</a></li>-<li><a href="/articles/flow-void">flow voids</a></li>-<li>vascular impressions</li>-<li>sphincteric contraction or <a href="/articles/pseudocalculus-sign-common-bile-duct">pseudocalculus sign</a>-</li>- +<li>
- +<p>MRCP specific potential pitfalls <sup>6</sup></p>
- +<ul>
- +<li><p><a href="/articles/magnetic-susceptibility-artifact">susceptibility artifacts</a></p></li>
- +<li><p><a href="/articles/flow-void">flow voids</a></p></li>
- +<li><p>vascular impressions</p></li>
- +<li><p>sphincteric contraction or <a href="/articles/pseudocalculus-sign-common-bile-duct">pseudocalculus sign</a></p></li>
References changed:
- 1. Sugiyama M, Suzuki Y, Abe N, Masaki T, Mori T, Atomi Y. Endoscopic Retreatment of Recurrent Choledocholithiasis After Sphincterotomy. Gut. 2004;53(12):1856-9. <a href="https://doi.org/10.1136/gut.2004.041020">doi:10.1136/gut.2004.041020</a> - <a href="https://www.ncbi.nlm.nih.gov/pubmed/15542528">Pubmed</a>
- 2. Borzellino G, Rodella L, Saladino E et al. Treatment for Retained [corrected] Common Bile Duct Stones During Laparoscopic Cholecystectomy: The Rendezvous Technique. Arch Surg. 2010;145(12):1145-9. <a href="https://doi.org/10.1001/archsurg.2010.261">doi:10.1001/archsurg.2010.261</a> - <a href="https://www.ncbi.nlm.nih.gov/pubmed/21173287">Pubmed</a>
- 3. Miller F, Hwang C, Gabriel H, Goodhartz L, Omar A, Parsons W. Contrast-Enhanced Helical CT of Choledocholithiasis. AJR Am J Roentgenol. 2003;181(1):125-30. <a href="https://doi.org/10.2214/ajr.181.1.1810125">doi:10.2214/ajr.181.1.1810125</a> - <a href="https://www.ncbi.nlm.nih.gov/pubmed/12818842">Pubmed</a>
- 4. Caoili E, Paulson E, Heyneman L, Branch M, Eubanks W, Nelson R. Helical CT Cholangiography with Three-Dimensional Volume Rendering Using an Oral Biliary Contrast Agent: Feasibility of a Novel Technique. AJR Am J Roentgenol. 2000;174(2):487-92. <a href="https://doi.org/10.2214/ajr.174.2.1740487">doi:10.2214/ajr.174.2.1740487</a> - <a href="https://www.ncbi.nlm.nih.gov/pubmed/10658729">Pubmed</a>
- 5. Adamek H, Albert J, Weitz M, Breer H, Schilling D, Riemann J. A Prospective Evaluation of Magnetic Resonance Cholangiopancreatography in Patients with Suspected Bile Duct Obstruction. Gut. 1998;43(5):680-3. <a href="https://doi.org/10.1136/gut.43.5.680">doi:10.1136/gut.43.5.680</a> - <a href="https://www.ncbi.nlm.nih.gov/pubmed/9824351">Pubmed</a>
- 6. Eugene Lin, Edward Escott, Kavita Garg et al. Practical Differential Diagnosis for CT and MRI. (2008) ISBN: 9781588906557 - <a href="http://books.google.com/books?vid=ISBN9781588906557">Google Books</a>
- 7. Chen W, Mo J, Lin L, Li C, Zhang J. Diagnostic Value of Magnetic Resonance Cholangiopancreatography in Choledocholithiasis. World J Gastroenterol. 2015;21(11):3351-60. <a href="https://doi.org/10.3748/wjg.v21.i11.3351">doi:10.3748/wjg.v21.i11.3351</a> - <a href="https://www.ncbi.nlm.nih.gov/pubmed/25805944">Pubmed</a>
- 8. Michael Maher, Adrian K. Dixon. Grainger & Allison's Diagnostic Radiology: Abdominal Imaging. (2015) ISBN: 9780702069383 - <a href="http://books.google.com/books?vid=ISBN9780702069383">Google Books</a>
- 1. Sugiyama M, Suzuki Y, Abe N et-al. Endoscopic retreatment of recurrent choledocholithiasis after sphincterotomy. Gut. 2004;53 (12): 1856-9. <a href="http://dx.doi.org/10.1136/gut.2004.041020">doi:10.1136/gut.2004.041020</a> - <a href="http://www.ncbi.nlm.nih.gov/pmc/articles/PMC1774317">Free text at pubmed</a> - <a href="http://www.ncbi.nlm.nih.gov/pubmed/15542528">Pubmed citation</a><div class="ref_v2"></div>
- 2. Borzellino G, Rodella L, Saladino E, Catalano F, Politi L, Minicozzi A, Cordiano C. Treatment for Retrieved Common Bile Duct Stones During Laparoscopic Cholecystectomy: The Rendezvous Technique. (2010) Archives of Surgery. 145 (12): 1145. <a href="https://doi.org/10.1001/archsurg.2010.261">doi:10.1001/archsurg.2010.261</a> <span class="ref_v4"></span>
- 3. Miller FH, Hwang CM, Gabriel H et-al. Contrast-enhanced helical CT of choledocholithiasis. AJR Am J Roentgenol. 2003;181 (1): 125-30. <a href="http://www.ajronline.org/cgi/content/full/181/1/125">AJR Am J Roentgenol (full text)</a> - <a href="http://www.ncbi.nlm.nih.gov/pubmed/12818842">Pubmed citation</a><div class="ref_v2"></div>
- 4. Caoili EM, Paulson EK, Heyneman LE et-al. Helical CT cholangiography with three-dimensional volume rendering using an oral biliary contrast agent: feasibility of a novel technique. AJR Am J Roentgenol. 2000;174 (2): 487-92. <a href="http://www.ajronline.org/cgi/content/full/174/2/487">AJR Am J Roentgenol (full text)</a> - <a href="http://www.ncbi.nlm.nih.gov/pubmed/10658729">Pubmed citation</a><div class="ref_v2"></div>
- 5. Adamek HE, Albert J, Weitz M et-al. A prospective evaluation of magnetic resonance cholangiopancreatography in patients with suspected bile duct obstruction. Gut. 1998;43 (5): 680-3. <a href="http://gut.bmj.com/cgi/pmidlookup?view=long&pmid=9824351">Gut (link)</a> - <a href="http://www.ncbi.nlm.nih.gov/pmc/articles/PMC1727306">Free text at pubmed</a> - <a href="http://www.ncbi.nlm.nih.gov/pubmed/9824351">Pubmed citation</a><div class="ref_v2"></div>
- 6. Lin E, Garg K, Escott E et-al. Practical differential diagnosis for CT and MRI. Thieme Medical Pub. (2008) ISBN:1588906558. <a href="http://books.google.com/books?vid=ISBN1588906558">Read it at Google Books</a> - <a href="http://www.amazon.com/gp/product/1588906558?ie=UTF8&tag=radiopaediaor-20&linkCode=as2&camp=1789&creative=9325&creativeASIN=1588906558">Find it at Amazon</a><div class="ref_v2"></div>
- 7. Chen W, Mo JJ, Lin L, Li CQ, Zhang JF. Diagnostic value of magnetic resonance cholangiopancreatography in choledocholithiasis. World journal of gastroenterology. 21 (11): 3351-60. <a href="https://doi.org/10.3748/wjg.v21.i11.3351">doi:10.3748/wjg.v21.i11.3351</a> - <a href="https://www.ncbi.nlm.nih.gov/pubmed/25805944">Pubmed</a> <span class="ref_v4"></span>
- 8. Michael Maher, Jr., Adrian K. Dixon. Grainger & Allison's Diagnostic Radiology: Abdominal Imaging. <a href="https://books.google.co.uk/books?vid=ISBN9780702069383">ISBN: 9780702069383</a><span class="ref_v4"></span>
Image ( destroy )
Image ( destroy )
Image ( destroy )
Image ( destroy )
Image ( destroy )
Image ( destroy )
Image ( destroy )
Image ( destroy )
Image ( destroy )
Image ( destroy )
Image ( destroy )
Image ( destroy )
Image ( destroy )
Image ( destroy )
Image ( destroy )
Image ( destroy )
Image ( destroy )
Image ( destroy )
Image ( destroy )
Image ( destroy )
Image ( destroy )
Image ( destroy )
Image ( destroy )
Image ( destroy )
Image ( destroy )
Image ( destroy )
Image ( destroy )
Image ( destroy )
Image ( destroy )
Image 1 MRI (T2) ( update )

Image 2 Fluoroscopy ( update )

Image 3 MRI (T2) ( update )

Image 4 Fluoroscopy ( update )

Image 5 MRI (T2) ( update )

Image 6 Ultrasound (Longitudinal) ( update )

Image 7 MRI (MRCP) ( update )

Image 8 ( update )

Image 9 MRI (T2 fat sat) ( update )

Image 10 Ultrasound (Longitudinal) ( update )

Image 11 MRI (T2 fat sat) ( update )
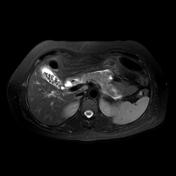
Image 12 CT (C+ portal venous phase) ( update )

Image 13 MRI (MRCP) ( update )

Image 14 CT (C+ portal venous phase) ( update )

Image 15 MRI (T2) ( update )
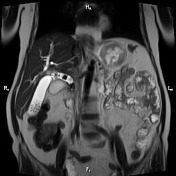
Image 16 Fluoroscopy (T-Tube cholangiography) ( update )

Image 17 MRI (MIP) ( update )

Image 18 CT (C+ portal venous phase) ( update )

Image 19 MRI (T2) ( update )

Image 20 Fluoroscopy (Frontal) ( update )

Image 21 MRI (T2) ( update )

Image 22 CT (C+ portal venous phase) ( update )








 Unable to process the form. Check for errors and try again.
Unable to process the form. Check for errors and try again.