Leigh syndrome
Updates to Article Attributes
Leigh disease,also known as subacute necrotizing encephalomyelopathy (SNEM), is a progressive neurodegenerative disorder and invariably leads to death in childhood.
Demographics and clinical presentation
Typically, symptoms become evident before the age of 2, with presentation in later childhood (juvenile form) or adulthood (adult form) being uncommon. Symptoms include 6:
- psychomotor delay
/ regression/regression - superimposed signs of basal ganglia and brain stem dysfunction
- ataxia
- ophthalmoplegia
- dystonia
- respiratory rhythm disturbance
- cranial nerve palsies
Genetics
The inheritance pattern may be either autosomal recessive or X linked.
Pathology
Leigh disease is one of many mitochondrial disorders, due to a wide variety of genetic mutations in mitochondrial DNA (mtDNA). As such it is only inherited from the mother, as is the case with other mitochondrial disorders. Some mutations (e.g. SURF 1) are particularly devastating 1.
Chronic energy deprivation leads to histological features such as 3:
- spongiform degeneration
- capillary proliferation
- demyelination
- neuronal loss
- gliosis
These findings are similar to those seen in infarction 4.
Markers
- CSF lactate may be elevated
Radiographic features
CT
CT demonstrates regions of low density matching areas of abnormal T2 signal on MRI (see below) 5. Occasionally some of these areas can demonstrate contrast enhancement 5.
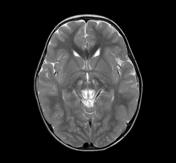
MRI
The distribution tends to be generally symmetrical.
-
T2:
-characterised by high signal typically in 3:- brainstem
- periaqueductal gray matter
- medulla
- midbrain
- putamen: characteristic but not always present 6
- other sites of T2 signal change include:
- remainder of the corpus striatum
([globus pallidus and caudate nucleus (heads))] - subthalamic nuclei
- substantia nigra
- thalami
- involvement of cerebral or cerebellar white matter is unusual 3.
- remainder of the corpus striatum
-
T1:
- usuallyusually demonstrates reduced signal in T2 abnormal areas, although some areas of hyperintensity can be seen, as can some enhancement. -
DWI:
- inin the acute setting some restricted diffusion may be evident. -
MR spectroscopy:
- featuresfeatures include- elevated choline
- occasionally elevated lactate
- reduced NAA
Treatment and prognosis
Prognosis is poor, with death usually occurring in childhood. The later the onset the slower the deterioration. Death is most frequently due to respiratory failure 6.
EtymologyHistory and etymology
It is named after Archibald Denis Leigh (Britith Neuropathologist) who first described the condition in 1951 2.
Differential diagnosis
-
Wernicke encephalopathy (WE)
- similar appearance but different demographics
- mammillary bodies not involved in Leigh disease
- enhancement more common in WE
- haemorrhagic change more common in WE 4
- other mitochondrial disorders
- brainstem and basal ganglia involvement less pronounced
-
acute necrotizing encephalitis of childhood
- lactate levels are usually normal
-<li>psychomotor delay / regression</li>- +<li>psychomotor delay/regression</li>
-</ul><p>These findings are similar to those seen in infarction <sup>4</sup>.</p><h5>Markers</h5><ul><li>CSF lactate may be elevated</li></ul><p> </p><h4>Radiographic features</h4><h5>CT</h5><p>CT demonstrates regions of low density matching areas of abnormal T2 signal on MRI (see below) <sup>5</sup>. Occasionally some of these areas can demonstrate contrast enhancement <sup>5</sup>.</p><h5>MRI</h5><p>The distribution tends to be generally symmetrical. </p><ul>- +</ul><p>These findings are similar to those seen in infarction <sup>4</sup>.</p><h5>Markers</h5><ul><li>CSF lactate may be elevated</li></ul><h4>Radiographic features</h4><h5>CT</h5><p>CT demonstrates regions of low density matching areas of abnormal T2 signal on MRI (see below) <sup>5</sup>. Occasionally some of these areas can demonstrate contrast enhancement <sup>5</sup>.</p><h5>MRI</h5><p>The distribution tends to be generally symmetrical. </p><ul>
-<strong>T2</strong> - characterised by high signal typically in <sup>3</sup>: <ul>- +<strong>T2:</strong> characterised by high signal typically in <sup>3</sup>: <ul>
-<li><a href="/articles/periaqueductal-gray-matter">periaqueductal gray matter</a></li>- +<li>periaqueductal gray matter</li>
-<a href="/articles/putamen">putamen </a>: characteristic but not always present <sup>6</sup>- +<a href="/articles/putamen">putamen</a>: characteristic but not always present <sup>6</sup>
-<li>remainder of the <a href="/articles/corpus-striatum">corpus striatum</a> (<a href="/articles/globus-pallidus">globus pallidus</a> and <a href="/articles/caudate-nucleus">caudate nucleus</a> (heads) )</li>- +<li>remainder of the <a href="/articles/corpus-striatum">corpus striatum</a> [<a href="/articles/globus-pallidus">globus pallidus</a> and <a href="/articles/caudate-nucleus">caudate nucleus</a> (heads)]</li>
-<strong>T1 </strong>- usually demonstrates reduced signal in T2 abnormal areas, although some areas of hyperintensity can be seen, as can some enhancement. </li>- +<strong>T1:</strong> usually demonstrates reduced signal in T2 abnormal areas, although some areas of hyperintensity can be seen, as can some enhancement. </li>
-<strong>DWI </strong>- in the acute setting some restricted diffusion may be evident.</li>- +<strong>DWI:</strong> in the acute setting some restricted diffusion may be evident.</li>
-<strong>MR spectroscopy</strong> - features include<ul>- +<strong>MR spectroscopy:</strong> features include<ul>
-</ul><p> </p><h4>Treatment and prognosis</h4><p>Prognosis is poor, with death usually occurring in childhood. The later the onset the slower the deterioration. Death is most frequently due to respiratory failure <sup>6</sup>.</p><h4><strong>Etymology</strong></h4><p>It is named after <strong>Archibald Denis</strong> <strong>Leigh</strong> (Britith Neuropathologist) who first described the condition in 1951 <sup>2</sup>.</p><h4>Differential diagnosis</h4><ul>- +</ul><h4>Treatment and prognosis</h4><p>Prognosis is poor, with death usually occurring in childhood. The later the onset the slower the deterioration. Death is most frequently due to respiratory failure <sup>6</sup>.</p><h4><strong>History and etymology</strong></h4><p>It is named after <strong>Archibald Denis</strong> <strong>Leigh</strong> (Britith Neuropathologist) who first described the condition in 1951 <sup>2</sup>.</p><h4>Differential diagnosis</h4><ul>
Image 1 MRI (T2) ( update )







 Unable to process the form. Check for errors and try again.
Unable to process the form. Check for errors and try again.