Osmotic demyelination syndrome
Updates to Article Attributes
Osmotic demyelination syndrome refers to acute demyelination seen in the setting of osmotic changes, typically with the rapid correction of hyponatraemia. It is the more recent term replacing central pontine myelinolysis, recognising that extrapontine structures can also be affected, previously known as extrapontine myelinolysis.
Epidemiology
The initial description of central pontine myelinolysis by Adams et al. in 1959 2 was entirely in a population of chronic alcoholics, and certainly, this scenario is common. Since then it has been increasingly recognised in other patient groups, but usually in the setting of rapidly corrected electrolyte disturbance 1:
- chronic alcoholics
- chronically debilitated patients
- transplant recipients
- pregnancy and hyperemesis
Clinical presentation
Clinically osmotic demyelination syndrome presents in a biphasic pattern. The first phase is usually attributable not to the demyelination but rather to the inciting electrolyte abnormality, with patients being acutely encephalopathic. Following rapid reversal of this abnormality, the patient transiently improves before progressing onto the classic osmotic demyelination syndrome features 2-3 days later. When pontine involvement is prominent, clinical features consist of:
- spastic quadriparesis
- pseudobulbar palsy
- changes in levels of consciousness
- coma
- death
Pathology
Although the exact mechanism is still uncertain, it is known that oligodendroglial cells are most susceptible to osmotic stresses, leading to their demise. It is not surprising that the distribution of osmotic myelinolysis, therefore, parallels the distribution of these cells.
Histologically, osmotic demyelination syndrome is characterised by intramyelinic splitting, vacuolation, and myelin sheath rupture 3. After many days, macrophages can be identified.
Radiographic features
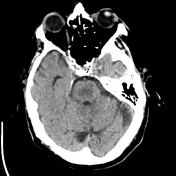
CT
CT may demonstrate low attenuation crossing the midline in the lower pons. However, CT assessment of the skull base can be difficult due to beam hardening artifact and, if available, MRI is preferred.
MRI
The earliest change is seen on DWI with restriction in the lower pons. This is seen within 24 hours of the onset of quadriplegia 3. This same region demonstrates eventual high T2 signal and later a low T1 signal. The T1 and T2 changes may take up to two weeks to develop. This region has a classic trident-shaped appearance. The overall appearance on T2/FLAIR axial MR images has also been likened to the face of a pig, referred to as piglet sign. Occasionally gadolinium enhancement is also demonstrated, just as in the acute phase of multiple sclerosis (MS) plaque. The peripheral fibres (ventrolateral longitudinal fibres, corticospinal tracts), as well as the periventricular and subpial regions, are typically spared.
Similar appearances are seen in other parts of the brain: basal ganglia, midbrain, and subcortical white matter.
Signal characteristics of the affected region include:
- T1: mildly or moderately hypointense
- T2/FLAIR: hyperintense, sparing the periphery and corticospinal tracts
- PD: hyperintense
- DWI: hyperintense
- ADC: signal low or signal loss
- T1 C+ (Gd): usually there is no enhancement, but some authors reported that it may occur 5,6
PET
Affected regions may demonstrate initial high uptake followed by subsequent low uptake with 18-FDG.
Treatment and prognosis
Some patients completely recover however six-month survival rate is only 5-10%.
Differential diagnosis
General imaging differential considerations include:
- demyelination including multiple sclerosis (MS)
- pontine infarction from basilar perforators can be central, although usually, brainstem infarcts stop at the midline
- pontine neoplasms including astrocytomas: brainstem is asymmetrically expanded with mass effect upon adjacent cisterns. local vessels may also be displaced
- brainstem metastasis: usually enhances
- vigabatrin toxicity: bilateral dorsal pontine longitudinal restricted diffusion
-<p><strong>Osmotic demyelination syndrome </strong>refers to acute <a href="/articles/demyelination">demyelination</a> seen in the setting of osmotic changes, typically with the rapid correction of <a href="/articles/hyponatremia">hyponatraemia</a>. It is the more recent term replacing <a href="/articles/central-pontine-myelinolysis-2">central pontine myelinolysis</a>, recognising that extrapontine structures can also be affected, previously known as <a href="/articles/extrapontine-myelinolysis-epm">extrapontine myelinolysis</a>. </p><h4>Epidemiology</h4><p>The initial description of central pontine myelinolysis by Adams et al. in 1959 <sup>2</sup> was entirely in a population of chronic alcoholics, and certainly, this scenario is common. Since then it has been increasingly recognised in other patient groups, but usually in the setting of rapidly corrected electrolyte disturbance <sup>1</sup>:</p><ul>-<li>chronic alcoholics</li>-<li>chronically debilitated patients</li>-<li>transplant recipients</li>-<li>pregnancy and hyperemesis</li>-</ul><h4>Clinical presentation</h4><p>Clinically osmotic demyelination syndrome presents in a biphasic pattern. The first phase is usually attributable not to the demyelination but rather to the inciting electrolyte abnormality, with patients being acutely encephalopathic. Following rapid reversal of this abnormality, the patient transiently improves before progressing onto the classic osmotic demyelination syndrome features 2-3 days later. When pontine involvement is prominent, clinical features consist of:</p><ul>-<li>spastic quadriparesis</li>-<li><a href="/articles/pseudobulbar-palsy">pseudobulbar palsy</a></li>-<li>changes in levels of consciousness</li>-<li>coma</li>-<li>death</li>-</ul><h4>Pathology</h4><p>Although the exact mechanism is still uncertain, it is known that oligodendroglial cells are most susceptible to osmotic stresses, leading to their demise. It is not surprising that the distribution of osmotic myelinolysis, therefore, parallels the distribution of these cells.</p><p>Histologically, osmotic demyelination syndrome is characterised by intramyelinic splitting, vacuolation, and myelin sheath rupture <sup>3</sup>. After many days, macrophages can be identified.</p><h4>Radiographic features</h4><h5>CT</h5><p>CT may demonstrate low attenuation crossing the midline in the lower <a href="/articles/pons">pons</a>. However, CT assessment of the skull base can be difficult due to <a href="/articles/beam-hardening">beam hardening artifact</a> and, if available, MRI is preferred.</p><h5>MRI</h5><p>The earliest change is seen on DWI with restriction in the lower pons. This is seen within 24 hours of the onset of quadriplegia <sup>3</sup>. This same region demonstrates eventual high T2 signal and later a low T1 signal. The T1 and T2 changes may take up to two weeks to develop. This region has a classic <a href="/articles/trident-sign-osmotic-demyelination">trident-shaped appearance</a>. The overall appearance on T2/FLAIR axial MR images has also been likened to the face of a pig, referred to as <a href="/articles/piglet-sign-osmotic-demyelination">piglet sign</a>. Occasionally gadolinium enhancement is also demonstrated, just as in the acute phase of <a href="/articles/multiple-sclerosis-ms">multiple sclerosis (MS</a><a href="/articles/multiple-sclerosis">)</a><a href="/articles/multiple-sclerosis-ms"> plaque</a>. The peripheral fibres (ventrolateral longitudinal fibres, <a href="/articles/corticospinal-tract">corticospinal tracts</a>), as well as the periventricular and subpial regions, are typically spared.</p><p>Similar appearances are seen in other parts of the brain: basal ganglia, midbrain, and subcortical white matter. </p><p>Signal characteristics of the affected region include:</p><ul>-<li>-<strong>T1</strong><strong>:</strong> mildly or moderately hypointense</li>-<li>-<strong>T2/FLAIR:</strong> hyperintense, sparing the periphery and <a href="/articles/anterior-corticospinal-tract">corticospinal tracts</a>-</li>-<li>-<strong>PD:</strong> hyperintense</li>-<li>-<strong>DWI:</strong> hyperintense</li>-<li>-<strong>ADC:</strong> signal low or signal loss</li>-<li>-<strong>T1 C+ (Gd):</strong> usually there is no enhancement, but some authors reported that it may occur <sup>5,6</sup>-</li>-</ul><h5>PET</h5><p>Affected regions may demonstrate initial high uptake followed by subsequent low uptake with 18-FDG.</p><h4>Treatment and prognosis</h4><p>Some patients completely recover however six-month survival rate is only 5-10%.</p><h4>Differential diagnosis</h4><p>General imaging differential considerations include:</p><ul>-<li>demyelination including <a href="/articles/multiple-sclerosis">multiple sclerosis (MS)</a>-</li>-<li>pontine infarction from basilar perforators can be central, although usually, <a href="/articles/brainstem">brainstem</a> infarcts stop at the midline</li>-<li>pontine neoplasms including <a href="/articles/astrocytic-tumours">astrocytomas</a>: <a href="/articles/brainstem-glioma">brainstem</a> is asymmetrically expanded with mass effect upon adjacent cisterns. local vessels may also be displaced</li>-<li>brainstem metastasis: usually enhances</li>-<li>vigabatrin toxicity: bilateral dorsal pontine longitudinal restricted diffusion</li>- +<p><strong>Osmotic demyelination syndrome </strong>refers to acute <a href="/articles/demyelination">demyelination</a> seen in the setting of osmotic changes, typically with the rapid correction of <a href="/articles/hyponatremia">hyponatraemia</a>. It is the more recent term replacing <a href="/articles/central-pontine-myelinolysis-2">central pontine myelinolysis</a>, recognising that extrapontine structures can also be affected, previously known as <a href="/articles/extrapontine-myelinolysis-epm">extrapontine myelinolysis</a>. </p><h4>Epidemiology</h4><p>The initial description of central pontine myelinolysis by Adams et al. in 1959 <sup>2</sup> was entirely in a population of chronic alcoholics, and certainly, this scenario is common. Since then it has been increasingly recognised in other patient groups, but usually in the setting of rapidly corrected electrolyte disturbance <sup>1</sup>:</p><ul>
- +<li>chronic alcoholics</li>
- +<li>chronically debilitated patients</li>
- +<li>transplant recipients</li>
- +<li>pregnancy and hyperemesis</li>
- +</ul><h4>Clinical presentation</h4><p>Clinically osmotic demyelination syndrome presents in a biphasic pattern. The first phase is usually attributable not to the demyelination but rather to the inciting electrolyte abnormality, with patients being acutely encephalopathic. Following rapid reversal of this abnormality, the patient transiently improves before progressing onto the classic osmotic demyelination syndrome features 2-3 days later. When pontine involvement is prominent, clinical features consist of:</p><ul>
- +<li>spastic quadriparesis</li>
- +<li><a href="/articles/pseudobulbar-palsy">pseudobulbar palsy</a></li>
- +<li>changes in levels of consciousness</li>
- +<li>coma</li>
- +<li>death</li>
- +</ul><h4>Pathology</h4><p>Although the exact mechanism is still uncertain, it is known that oligodendroglial cells are most susceptible to osmotic stresses, leading to their demise. It is not surprising that the distribution of osmotic myelinolysis, therefore, parallels the distribution of these cells.</p><p>Histologically, osmotic demyelination syndrome is characterised by intramyelinic splitting, vacuolation, and myelin sheath rupture <sup>3</sup>. After many days, macrophages can be identified.</p><h4>Radiographic features</h4><h5>CT</h5><p>CT may demonstrate low attenuation crossing the midline in the lower <a href="/articles/pons">pons</a>. However, CT assessment of the skull base can be difficult due to <a href="/articles/beam-hardening">beam hardening artifact</a> and, if available, MRI is preferred.</p><h5>MRI</h5><p>The earliest change is seen on DWI with restriction in the lower pons. This is seen within 24 hours of the onset of quadriplegia <sup>3</sup>. This same region demonstrates eventual high T2 signal and later a low T1 signal. The T1 and T2 changes may take up to two weeks to develop. This region has a classic <a href="/articles/trident-sign-osmotic-demyelination">trident-shaped appearance</a>. The overall appearance on T2/FLAIR axial MR images has also been likened to the face of a pig, referred to as <a href="/articles/piglet-sign-osmotic-demyelination">piglet sign</a>. Occasionally gadolinium enhancement is also demonstrated, just as in the acute phase of <a href="/articles/multiple-sclerosis-ms">multiple sclerosis (MS</a><a href="/articles/multiple-sclerosis">)</a><a href="/articles/multiple-sclerosis-ms"> plaque</a>. The peripheral fibres (ventrolateral longitudinal fibres, <a href="/articles/corticospinal-tract">corticospinal tracts</a>), as well as the periventricular and subpial regions, are typically spared.</p><p>Similar appearances are seen in other parts of the brain: basal ganglia, midbrain, and subcortical white matter. </p><p>Signal characteristics of the affected region include:</p><ul>
- +<li>
- +<strong>T1</strong><strong>:</strong> mildly or moderately hypointense</li>
- +<li>
- +<strong>T2/FLAIR:</strong> hyperintense, sparing the periphery and <a href="/articles/anterior-corticospinal-tract">corticospinal tracts</a>
- +</li>
- +<li>
- +<strong>PD:</strong> hyperintense</li>
- +<li>
- +<strong>DWI:</strong> hyperintense</li>
- +<li>
- +<strong>ADC:</strong> signal low or signal loss</li>
- +<li>
- +<strong>T1 C+ (Gd):</strong> usually there is no enhancement, but some authors reported that it may occur <sup>5,6</sup>
- +</li>
- +</ul><h5>PET</h5><p>Affected regions may demonstrate initial high uptake followed by subsequent low uptake with 18-FDG.</p><h4>Treatment and prognosis</h4><p>Some patients completely recover however six-month survival rate is only 5-10%.</p><h4>Differential diagnosis</h4><p>General imaging differential considerations include:</p><ul>
- +<li>demyelination including <a href="/articles/multiple-sclerosis">multiple sclerosis (MS)</a>
- +</li>
- +<li>pontine infarction from basilar perforators can be central, although usually, <a href="/articles/brainstem">brainstem</a> infarcts stop at the midline</li>
- +<li>pontine neoplasms including <a href="/articles/astrocytic-tumours">astrocytomas</a>: <a href="/articles/brainstem-glioma">brainstem</a> is asymmetrically expanded with mass effect upon adjacent cisterns. local vessels may also be displaced</li>
- +<li>brainstem metastasis: usually enhances</li>
- +<li>vigabatrin toxicity: bilateral dorsal pontine longitudinal restricted diffusion</li>
Image 15 CT (non-contrast) ( update )







 Unable to process the form. Check for errors and try again.
Unable to process the form. Check for errors and try again.