Subdural hemorrhage (summary)
Updates to Article Attributes
- this is a basic article for medical students and non-radiologists
- for more information, see the main Subdural haemorrhage article
Subdural haemorrhage (SDH) is a collection of blood between the dura and the arachnoid layers of the meninges. They are common (15% of all head injuries) and can occur in any age range. There is usually a history of head trauma and prognosis can depend on the extent of the bleed.
Epidemiology
Subdural haemorrhages can occur across many ages, but with different mechanisms at different ages:
- children: non-accidental injury
- adults: high energy trauma (e.g. road traffic collisions)
- elderly: falls (there may not be a clear history of trauma)
Clinical presentation
Acute subdurals are usually associated with head injury - particularly in younger patients with other evidence of head injury (extradural haemorrhages, cerebral contusions). There may be underlying abnormalities such as arteriovenous malformations in spontaneous bleeds.
Subacute or chronic subdural haemorrhages can present in the elderly on CT as part of confusion screens or following vague neurological changes. SDH is a classic cause of pseudo-dementia and there may be minor or no head injury in the history.
Pathophysiology
The bleed in subdural haemorrhages usually comes from "bridging veins" found in the subdural space (from the cortex to dural sinuses). These veins can be subject to shearing or tearing when the head is subject to a change in velocity (as in head injury). These can be more prevalent in the elderly where the effect of cerebral atrophy can leave these stretched veins more vulnerable to damage.
There can also be leaking of CSF into the subdural space if the underlying arachnoid mater is damaged. A minority can also rebleed as further veins are stretched.
Radiographic features
Subdural haemorrhages are typically unilateral (85%) and follow a crescent-like distribution around the periphery of the brain. They are not limited by sutures but instead can fill to dural reflections (falx cerebri, tentorium and falx cerebelli). Common sites are the middles cranial fossa and fronto-parietal convexities.
CT
Non-contrast CT is usually enough to make the diagnosis but contrast can be used in challenging cases, particularly with the different appearances of these bleeds over time.
Hyperacute
It is unlikely that most patients will be imaged in the first hour of the bleed but these SDHs can appear isodense with a swirl sign as the blood products enter the subdural space. In cases of head trauma, there may be other radiographic evidence (fractures, oedema) which can add to the mass effect.
Acute
Acute subdural haemorrhages appear as hyperdense, uniform collections. They are hyperdense to brain parenchyma as the clot collects and retracts.
Up to half can have mixed appearances as unclotted blood, serum of CSF is involved in the collection and appear hypo-dense.
In a few cases, acute bleeds can be isodense and difficult to identify. This can be the case in patients with anaemia or coagulopathies (including warfarinisation) as "hyperdense" clots have difficulty forming.
Subacute
In the first few weeks after a bleed, the clot and proteins can be broken down making the collection appear hypo- or isodense. Here, indirect signs such as a gap between the cerebral sulci and skull, mass effect or an illdefined, thickened appearance to the cortex.
Chronic
Over time, these collections can resolve and leave few products behind with a hypodense area on scans (similar to CSF).
MRI
MRI can also be used to determine the chronicity of subdural haemorrhages using T1, T2 and FLAIR sequences. This is detailed on the main Subdural haemorrhage page.
Treatment and prognosis
Subdural haemorrhages usual merit discuss with neurosurgical services. The treatment can depend on the neurological impact of the mass effect and size of the bleed.
Small chronic SDHs may be incidental findings and can be observed with repeated scans.
Correction of abnormal coagulation can be performed prior to neurosurgical intervention with haematologist advice. Evacuation of the bleed is usually required in symptomatic cases - but can carry high morbidity and mortality. Acute SDHs may need urgent craniotomy to control the clot. Symptomatic subacute or chronic clots can be managed with burr-hole drainage as the older clots can be more easily removed from smaller spaces.
Differential diagnosis
- Subdural empyema - similar appearance on CT scans but usually febrile and generally unwell, can enhance with contrast with evidence of abscess or underlying infarction
- EDH (basic) - difficult if small to differentiate, EDH are bi-convex rather than crescentic, EDH limited by sutures, SDH by dural reflections, usually clear history of head trauma/skull fracture
- Subdural hygroma - very similar appearance of CT, same density as CSF, no evidence of previous haemorrhage
- enlarged subarachnoid space (due to cerebral atrophy or changes in infancy)
- scan motion artefact
-</ul><h4>Clinical presentation</h4><p>Acute subdurals are usually associated with head injury - particularly in younger patients with other evidence of head injury (extradural haemorrhages, cerebral contusions). There may be underlying abnormalities such as arteriovenous malformations in spontaneous bleeds.</p><p>Subacute or chronic subdural haemorrhages can present in the elderly on CT as part of confusion screens or following vague neurological changes. SDH is a classic cause of pseudo-dementia and there may be minor or no head injury in the history.</p><h4>Pathophysiology</h4><p>The bleed in subdural haemorrhages usually comes from "bridging veins" found in the subdural space (from the cortex to dural sinuses). These veins can be subject to shearing or tearing when the head is subject to a change in velocity (as in head injury). These can be more prevalent in the elderly where the effect of cerebral atrophy can leave these stretched veins more vulnerable to damage.</p><p>There can also be leaking of CSF into the subdural space if the underlying arachnoid mater is damaged. A minority can also rebleed as further veins are stretched.</p><h4>Radiographic features</h4><p>Subdural haemorrhages are typically unilateral (85%) and follow a crescent-like distribution around the periphery of the brain. They are not limited by sutures but instead can fill to dural reflections (falx cerebri, tentorium and falx cerebelli). Common sites are the middles cranial fossa and fronto-parietal convexities.</p><h5>CT</h5><p>Non-contrast CT is usually enough to make the diagnosis but contrast can be used in challenging cases, particularly with the different appearances of these bleeds over time.</p><h6>Hyperacute</h6><p>It is unlikely that most patients will be imaged in the first hour of the bleed but these SDHs can appear isodense with a swirl sign as the blood products enter the subdural space. In cases of head trauma, there may be other radiographic evidence (fractures, oedema) which can add to the mass effect.</p><h6>Acute</h6><p>Acute subdural haemorrhages appear as hyperdense, uniform collections. They are hyperdense to brain parenchyma as the clot collects and retracts.</p><p>Up to half can have mixed appearances as unclotted blood, serum of CSF is involved in the collection and appear hypo-dense.</p><p>In a few cases, acute bleeds can be isodense and difficult to identify. This can be the case in patients with anaemia or coagulopathies (including warfarinisation) as "hyperdense" clots have difficulty forming.</p><h6>Subacute</h6><p>In the first few weeks after a bleed, the clot and proteins can be broken down making the collection appear hypo- or isodense. Here, indirect signs such as a gap between the cerebral sulci and skull, mass effect or an illdefined, thickened appearance to the cortex.</p><h6>Chronic</h6><p>Over time, these collections can resolve and leave few products behind with a hypodense area on scans (similar to CSF).</p><h5>MRI</h5><p>MRI can also be used to determine the chronicity of subdural haemorrhages using T1, T2 and FLAIR sequences. This is detailed on the main <a href="/articles/subdural-haemorrhage">Subdural haemorrhage</a> page.</p><h4>Treatment and prognosis</h4><p>Subdural haemorrhages usual merit discuss with neurosurgical services. The treatment can depend on the neurological impact of the mass effect and size of the bleed.</p><p>Small chronic SDHs may be incidental findings and can be observed with repeated scans.</p><p>Correction of abnormal coagulation can be performed prior to neurosurgical intervention with haematologist advice. Evacuation of the bleed is usually required in symptomatic cases - but can carry high morbidity and mortality. Acute SDHs may need urgent craniotomy to control the clot. Symptomatic subacute or chronic clots can be managed with burr-hole drainage as the older clots can be more easily removed from smaller spaces.</p><h4>Differential diagnosis</h4><p> </p>- +</ul><h4>Clinical presentation</h4><p>Acute subdurals are usually associated with head injury - particularly in younger patients with other evidence of head injury (extradural haemorrhages, cerebral contusions). There may be underlying abnormalities such as arteriovenous malformations in spontaneous bleeds.</p><p>Subacute or chronic subdural haemorrhages can present in the elderly on CT as part of confusion screens or following vague neurological changes. SDH is a classic cause of pseudo-dementia and there may be minor or no head injury in the history.</p><h4>Pathophysiology</h4><p>The bleed in subdural haemorrhages usually comes from "bridging veins" found in the subdural space (from the cortex to dural sinuses). These veins can be subject to shearing or tearing when the head is subject to a change in velocity (as in head injury). These can be more prevalent in the elderly where the effect of cerebral atrophy can leave these stretched veins more vulnerable to damage.</p><p>There can also be leaking of CSF into the subdural space if the underlying arachnoid mater is damaged. A minority can also rebleed as further veins are stretched.</p><h4>Radiographic features</h4><p>Subdural haemorrhages are typically unilateral (85%) and follow a crescent-like distribution around the periphery of the brain. They are not limited by sutures but instead can fill to dural reflections (falx cerebri, tentorium and falx cerebelli). Common sites are the middles cranial fossa and fronto-parietal convexities.</p><h5>CT</h5><p>Non-contrast CT is usually enough to make the diagnosis but contrast can be used in challenging cases, particularly with the different appearances of these bleeds over time.</p><h6>Hyperacute</h6><p>It is unlikely that most patients will be imaged in the first hour of the bleed but these SDHs can appear isodense with a swirl sign as the blood products enter the subdural space. In cases of head trauma, there may be other radiographic evidence (fractures, oedema) which can add to the mass effect.</p><h6>Acute</h6><p>Acute subdural haemorrhages appear as hyperdense, uniform collections. They are hyperdense to brain parenchyma as the clot collects and retracts.</p><p>Up to half can have mixed appearances as unclotted blood, serum of CSF is involved in the collection and appear hypo-dense.</p><p>In a few cases, acute bleeds can be isodense and difficult to identify. This can be the case in patients with anaemia or coagulopathies (including warfarinisation) as "hyperdense" clots have difficulty forming.</p><h6>Subacute</h6><p>In the first few weeks after a bleed, the clot and proteins can be broken down making the collection appear hypo- or isodense. Here, indirect signs such as a gap between the cerebral sulci and skull, mass effect or an illdefined, thickened appearance to the cortex.</p><h6>Chronic</h6><p>Over time, these collections can resolve and leave few products behind with a hypodense area on scans (similar to CSF).</p><h5>MRI</h5><p>MRI can also be used to determine the chronicity of subdural haemorrhages using T1, T2 and FLAIR sequences. This is detailed on the main <a href="/articles/subdural-haemorrhage">Subdural haemorrhage</a> page.</p><h4>Treatment and prognosis</h4><p>Subdural haemorrhages usual merit discuss with neurosurgical services. The treatment can depend on the neurological impact of the mass effect and size of the bleed.</p><p>Small chronic SDHs may be incidental findings and can be observed with repeated scans.</p><p>Correction of abnormal coagulation can be performed prior to neurosurgical intervention with haematologist advice. Evacuation of the bleed is usually required in symptomatic cases - but can carry high morbidity and mortality. Acute SDHs may need urgent craniotomy to control the clot. Symptomatic subacute or chronic clots can be managed with burr-hole drainage as the older clots can be more easily removed from smaller spaces.</p><h4>Differential diagnosis</h4><ul>
- +<li>
- +<a href="/articles/subdural-empyema">Subdural empyema</a> - similar appearance on CT scans but usually febrile and generally unwell, can enhance with contrast with evidence of abscess or underlying infarction</li>
- +<li>
- +<a href="/articles/extradural-haemorrhage-basic">EDH (basic)</a> - difficult if small to differentiate, EDH are bi-convex rather than crescentic, EDH limited by sutures, SDH by dural reflections, usually clear history of head trauma/skull fracture</li>
- +<li>
- +<a href="/articles/subdural-hygroma">Subdural hygroma</a> - very similar appearance of CT, same density as CSF, no evidence of previous haemorrhage</li>
- +<li>enlarged subarachnoid space (due to cerebral atrophy or changes in infancy)</li>
- +<li>scan motion artefact</li>
- +</ul>
Tags changed:
- sdh
- subdural haemorrhage
- subdural haematoma
Systems changed:
- Central Nervous System
Image ( create )
Image 1 Diagram ( create )

Image 2 CT (non-contrast) ( create )
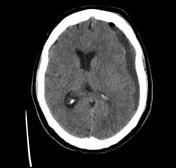
Image 4 CT (non-contrast) ( create )

Image 5 CT (non-contrast) ( create )

Image 6 CT (non-contrast) ( create )

Image 7 CT (non-contrast) ( create )

Image 8 CT (non-contrast) ( create )








 Unable to process the form. Check for errors and try again.
Unable to process the form. Check for errors and try again.