Thyroid-associated orbitopathy
Updates to Article Attributes
Thyroid associated orbitopathy (TAO) is the most common cause of proptosis in adults 1, and is most frequently associated with Graves disease.
Epidemiology
The demographics of thyroid associated orbitopathy reflects that of patients with thyroid disease, and is therefore more frequently seen in women. Although Graves disease is the most common cause, Hashimoto thyroiditis has also been implicated. It may precede, occur concurrently with, or after onset of abnormal thyroid function.
Clinical presentation
Clinical presentation includes 1:
- lid-retraction
- proptosis, with resultant chemosis and corneal dryness and ulceration
- optic nerve compression potentially leading to blindness
- diplopia
Pathology
Thyroid associated orbitopathy is characterised by enlargement of the extraocular muscles (EOMs) as well as increase in the orbital fat volume 1. While the exact mechanism is unknown, antibodies to thyroid stimulating hormone (TSH) appear to cross react with antigens in the orbit resulting in infiltration by activated T lymphocytes 3, with subsequent release of inflammatory mediators.
The muscles are infiltrated with inflammatory cells (lymphocytes, macrophages, plasma cells and eosinophils), and increased mucopolysccaride deposition. In long standing cases increased collagen deposition leads to fibrosis 1.
Increase in orbital fat volume is as a result of venous congestion (compression of superior ophthalmic vein by enlarged muscles) and / or intrinsic inflammation.
The extra-ocular muscles are involved in a predictable fashion as remembered by the I'M SLOW mnemonic. Involvement of the rectus muscles in decreasing order of frequency:
- inferior
- medial
- superior
- lateral
- obliques
Radiographic features
CT
CT is the most commonly used modality, due to its widespread availability and rapid image acquisition. Contrast, although ideal, is not necessary as the natural contrast between orbital fat and muscle allows for adequate delineation of the orbital content.
The order of extraocular muscle involvement can be remembered by the mnemonic I'M SLOW, and bilateral (76-90%) and symmetric (70%) involvement is typical. The tendon is typically spared (although it can be involved in acute cases) with the swelling largely confined to the muscle belly. This appearance if often referred to as 'coke bottle' in nature (coca-cola bottle sign), given its resemblance to the classic coca-cola bottle.
When muscle involvement is pronounced the optic nerve may be crowded at the orbital apex, leading to optic nerve dysfunction 1. Variation in the shape of the orbit, especially the angle formed by the medial and lateral walls at the apex, changes the likelihood of optic nerve compression 2.
MRI
MRI may also be used in evaluation due to its multiplanar and the inherent contrast capabilities. Use of MR prevents ionizing radiation to orbits. The imaging findings are similar as described above for CT in terms of location and ocular muscles involved.
Treatment and prognosis
Although in many instances the disease is self limiting, spontaneously improving within 2-5 years 3 often discomfort, cosmetic issues, the risk of corneal ulceration and optic nerve compression requires treatment. Options include :
- medical - supportive, steroids
- radiotherapy 3
- surgical decompression
Differential diagnosis
General imaging differential considerations include
-<p><strong>Thyroid associated orbitopathy (TAO)</strong> is the most common cause of proptosis in adults <sup>1</sup>, and is most frequently associated with <a href="/articles/graves-disease">Graves disease</a>.</p>-<h4>Epidemiology</h4>-<p>The demographics of thyroid associated orbitopathy reflects that of patients with thyroid disease, and is therefore more frequently seen in women. Although <a title="Graves disease" href="/articles/graves-disease">Graves disease</a> is the most common cause, <a href="/articles/hashimoto-thyroiditis">Hashimoto thyroiditis</a> has also been implicated. It may precede, occur concurrently with, or after onset of abnormal thyroid function. </p>-<h4>Clinical presentation</h4>-<p>Clinical presentation includes <sup>1</sup>:</p>-<ul>-<li>lid-retraction</li>-<li>proptosis, with resultant chemosis and corneal dryness and ulceration </li>-<li>optic nerve compression potentially leading to blindness </li>-<li>diplopia </li>-</ul><h4>Pathology</h4>-<p>Thyroid associated orbitopathy is characterised by enlargement of the <a title="extraocular muscles" href="/articles/extra-ocular-muscles">extraocular muscles</a> (EOMs) as well as increase in the orbital fat volume <sup>1</sup>. While the exact mechanism is unknown, antibodies to <a title="thyroid stimulating hormone" href="/articles/thyroid-stimulating-hormone">thyroid stimulating hormone</a> (TSH) appear to cross react with antigens in the orbit resulting in infiltration by activated T lymphocytes <sup>3</sup>, with subsequent release of inflammatory mediators. </p>-<p>The muscles are infiltrated with inflammatory cells (lymphocytes, macrophages, plasma cells and eosinophils), and increased mucopolysccaride deposition. In long standing cases increased collagen deposition leads to fibrosis <sup>1</sup>. </p>-<p>Increase in orbital fat volume is as a result of venous congestion (compression of <a title="superior ophthalmic vein" href="/articles/superior-ophthalmic-vein">superior ophthalmic vein</a> by enlarged muscles) and / or intrinsic inflammation. </p>-<p>The <a title="extra-ocular muscle" href="/articles/extra-ocular-muscles">extra-ocular muscles</a> are involved in a predictable fashion as remembered by the <a title="I'M SLOW" href="/articles/extraocular-muscle-involvement-in-thyroid-associated-orbitopathy-mnemonic">I'M SLOW</a> mnemonic. Involvement of the rectus muscles in decreasing order of frequency:</p>-<ul>-<li>inferior</li>-<li>medial</li>-<li>superior</li>-<li>lateral</li>-<li>obliques</li>-</ul><h4>Radiographic features</h4>-<h5>CT</h5>-<p>CT is the most commonly used modality, due to its widespread availability and rapid image acquisition. Contrast, although ideal, is not necessary as the natural contrast between orbital fat and muscle allows for adequate delineation of the orbital content. </p>-<p>The order of extraocular muscle involvement can be remembered by the mnemonic <a title="I'M SLOW" href="/articles/extraocular-muscle-involvement-in-thyroid-associated-orbitopathy-mnemonic">I'M SLOW</a>, and bilateral (76-90%) and symmetric (70%) involvement is typical. The tendon is typically spared (although it can be involved in acute cases) with the swelling largely confined to the muscle belly. This appearance if often referred to as 'coke bottle' in nature (<a title="Coca-Cola bottle sign" href="/articles/coca-cola-bottle-sign">coca-cola bottle sign</a>), given its resemblance to the classic coca-cola bottle.</p>-<p>When muscle involvement is pronounced the <a href="/articles/optic-nerve">optic nerve</a> may be crowded at the <a title="orbital apex" href="/articles/orbital-apex">orbital apex</a>, leading to optic nerve dysfunction <sup>1</sup>. Variation in the shape of the orbit, especially the angle formed by the medial and lateral walls at the apex, changes the likelihood of <a title="optic nerve compression" href="/articles/optic-nerve-compression">optic nerve compression</a> <sup>2</sup>.</p>-<h5>MRI</h5>-<p>MRI may also be used in evaluation due to its multiplanar and the inherent contrast capabilities. Use of MR prevents ionizing radiation to orbits. The imaging findings are similar as described above for CT in terms of location and ocular muscles involved.</p><a name="Treatment"></a>-<h4><span>Treatment and prognosis</span></h4>-<p>Although in many instances the disease is self limiting, spontaneously improving within 2-5 years <sup>3</sup> often discomfort, cosmetic issues, the risk of corneal ulceration and optic nerve compression requires treatment. Options include :</p>-<ul>-<li>medical - supportive, steroids</li>- +<p><strong>Thyroid associated orbitopathy (TAO)</strong> is the most common cause of proptosis in adults <sup>1</sup>, and is most frequently associated with <a href="/articles/graves-disease">Graves disease</a>.</p><h4>Epidemiology</h4><p>The demographics of thyroid associated orbitopathy reflects that of patients with thyroid disease, and is therefore more frequently seen in women. Although <a href="/articles/graves-disease">Graves disease</a> is the most common cause, <a href="/articles/hashimoto-thyroiditis">Hashimoto thyroiditis</a> has also been implicated. It may precede, occur concurrently with, or after onset of abnormal thyroid function.</p><h4>Clinical presentation</h4><p>Clinical presentation includes <sup>1</sup>:</p><ul>
- +<li>lid-retraction</li>
- +<li>proptosis, with resultant chemosis and corneal dryness and ulceration</li>
- +<li>optic nerve compression potentially leading to blindness</li>
- +<li>diplopia</li>
- +</ul><h4>Pathology</h4><p>Thyroid associated orbitopathy is characterised by enlargement of the <a href="/articles/extra-ocular-muscles">extraocular muscles</a> (EOMs) as well as increase in the orbital fat volume <sup>1</sup>. While the exact mechanism is unknown, antibodies to <a href="/articles/thyroid-stimulating-hormone">thyroid stimulating hormone</a> (TSH) appear to cross react with antigens in the orbit resulting in infiltration by activated T lymphocytes <sup>3</sup>, with subsequent release of inflammatory mediators.</p><p>The muscles are infiltrated with inflammatory cells (lymphocytes, macrophages, plasma cells and eosinophils), and increased mucopolysccaride deposition. In long standing cases increased collagen deposition leads to fibrosis <sup>1</sup>. </p><p>Increase in orbital fat volume is as a result of venous congestion (compression of <a href="/articles/superior-ophthalmic-vein">superior ophthalmic vein</a> by enlarged muscles) and / or intrinsic inflammation.</p><p>The <a href="/articles/extra-ocular-muscles">extra-ocular muscles</a> are involved in a predictable fashion as remembered by the <a href="/articles/extraocular-muscle-involvement-in-thyroid-associated-orbitopathy-mnemonic">I'M SLOW</a> mnemonic. Involvement of the rectus muscles in decreasing order of frequency:</p><ul>
- +<li>inferior</li>
- +<li>medial</li>
- +<li>superior</li>
- +<li>lateral</li>
- +<li>obliques</li>
- +</ul><h4>Radiographic features</h4><h5>CT</h5><p>CT is the most commonly used modality, due to its widespread availability and rapid image acquisition. Contrast, although ideal, is not necessary as the natural contrast between orbital fat and muscle allows for adequate delineation of the orbital content.</p><p>The order of extraocular muscle involvement can be remembered by the mnemonic <a href="/articles/extraocular-muscle-involvement-in-thyroid-associated-orbitopathy-mnemonic">I'M SLOW</a>, and bilateral (76-90%) and symmetric (70%) involvement is typical. The tendon is typically spared (although it can be involved in acute cases) with the swelling largely confined to the muscle belly. This appearance if often referred to as 'coke bottle' in nature (<a href="/articles/coca-cola-bottle-sign">coca-cola bottle sign</a>), given its resemblance to the classic coca-cola bottle.</p><p>When muscle involvement is pronounced the <a href="/articles/optic-nerve">optic nerve</a> may be crowded at the <a href="/articles/orbital-apex">orbital apex</a>, leading to optic nerve dysfunction <sup>1</sup>. Variation in the shape of the orbit, especially the angle formed by the medial and lateral walls at the apex, changes the likelihood of <a href="/articles/optic-nerve-compression">optic nerve compression</a> <sup>2</sup>.</p><h5>MRI</h5><p>MRI may also be used in evaluation due to its multiplanar and the inherent contrast capabilities. Use of MR prevents ionizing radiation to orbits. The imaging findings are similar as described above for CT in terms of location and ocular muscles involved.</p><p> </p><h4>Treatment and prognosis</h4><p>Although in many instances the disease is self limiting, spontaneously improving within 2-5 years <sup>3</sup> often discomfort, cosmetic issues, the risk of corneal ulceration and optic nerve compression requires treatment. Options include :</p><ul>
- +<li>medical - supportive, steroids</li>
-</li>-<li>surgical decompression</li>-</ul><a name="Differential_diagnosis"></a>-<h4><span>Differential diagnosis</span></h4>-<p><span>General imaging differential considerations include</span></p>-<ul>-<li>-<a title="Orbital pseudotumour" href="/articles/orbital_pseudotumour">orbital pseudotumour</a><a title="Orbital pseudotumour" href="/articles/orbital_pseudotumour"></a> </li>-<li><a title="Orbital sarcoidosis" href="/articles/orbital-sarcoidosis">orbital sarcoidosis</a></li>-<li><a title="Orbital lymphoma" href="/articles/orbital-lymphoma">orbital lymphoma</a></li>-<li><a title="Orbital metastases" href="/articles/orbital-metastases">orbital metastases</a></li>-<li><a title="orbital amyloidosis" href="/articles/orbital-amyloidosis">orbital amyloidosis</a></li>-<li><a title="Erdheim-Chester Disease" href="/articles/erdheim-chester_disease">Erdheim Chester disease</a></li>- +</li>
- +<li>surgical decompression</li>
- +</ul><p> </p><h4>Differential diagnosis</h4><p>General imaging differential considerations include</p><ul>
- +<li><a href="/articles/orbital-pseudotumour">orbital pseudotumour</a></li>
- +<li><a href="/articles/orbital-sarcoidosis">orbital sarcoidosis</a></li>
- +<li><a href="/articles/orbital-lymphoma">orbital lymphoma</a></li>
- +<li><a href="/articles/orbital-metastases">orbital metastases</a></li>
- +<li><a href="/articles/orbital-amyloidosis">orbital amyloidosis</a></li>
- +<li><a href="/articles/erdheim-chester-disease">Erdheim Chester disease</a></li>
Image ( update )
Image ( update )
Image 1 CT (non-contrast) ( update )
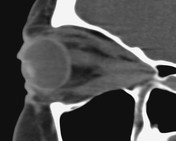
Image 2 CT (non-contrast) ( update )

Image 5 CT (C+ delayed) ( update )

Image 10 MRI (T1) ( update )

Image 12 CT (non-contrast) ( create )








 Unable to process the form. Check for errors and try again.
Unable to process the form. Check for errors and try again.