Radiopaedia.org is fundamentally about facilitating access to quality radiology teaching material, so that medical professionals from around the world can better diagnose and treat their patients. I believe it is crucial that such access is not determined by the wealth of your country or that of your institution.
Unfortunately much of the medical education industry (journals, textbooks, courses and meetings) functions primarily by directly monetizing access to this information. Although we have made great inroads in creating a free resource of thousands of articles and cases, we recognize the importance of meetings where an expert can guide you through the diagnostic process. This is one of the reasons why we have started running Radiopaedia Courses and making these course as easily available as possible. We can't do it all on our own however.
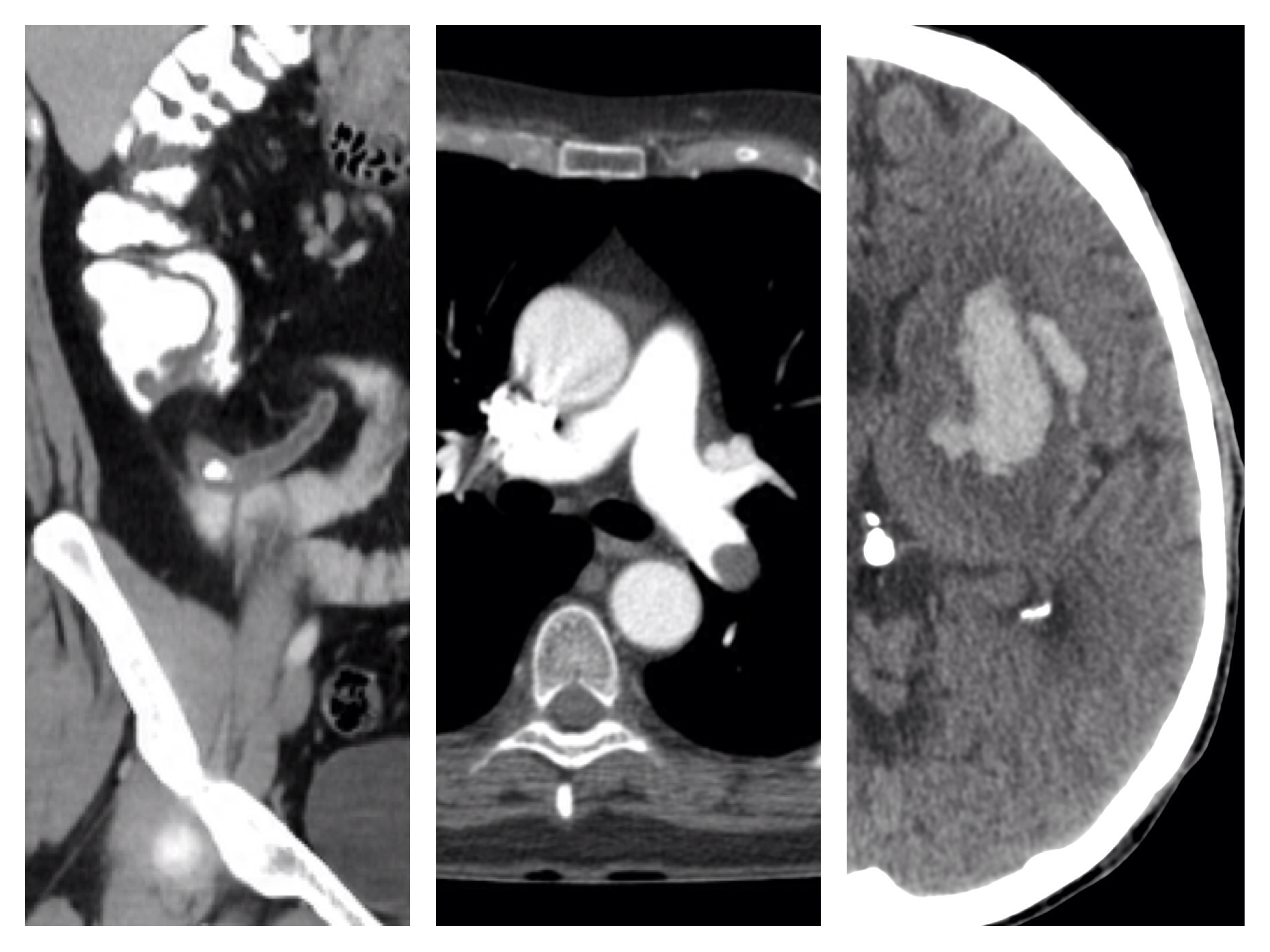
Thus, when I was approached by the organizing committee of ANZSNR 2015 (Australian and New Zealand Society of Neuroradiology - March 21-22 - Melbourne, Australia) to help bring at least some of the meeting to the world, I was wrapped. Together with my colleagues A.Prof Peter Mitchell, A.Prof Pramit Phal and Dr Christine Goh, we will be presenting over 5 hours of case-based learning, covering the spine, cerebrovascular conditions, pitutiary region, tumors and tumor like conditions, and neurodegenerative diseases.
I have had the pleasure of learning a great deal from all my fellow speakers over the years, and can say without equivocation that watching them explain their approach to a case and how they narrow down a differential is an exceptional way to learn.
It is therefore with great pleasure that we can share with you over 100 of the cases that we will be presenting and discussing at the meeting. Radiology is not about the answer, so much as the process, so feel free to read through these cases ahead of the meeting.
For those of you not able to attend, I hope you will gain a great deal from this collection of curated cases, and that you won't feel too bad about missing out on the live event; there is always next year. :)
In addition to accessing these cases through your browser (on any computer or device), we have also created a bespoke iOS (iPhone / iPad).
To find the app (free) just follow this link, or merely search for "ANZSNR" in the App Store.
To view the cases within Radiopaedia.org, follow (and bookmark) the links below.
If you are lucky enough to be able to attend ANZSNR 2015 (meeting details here), and you see me milling about, please come up and say hi and let me know what you think of the app / cases.
Frank Gaillard










 Unable to process the form. Check for errors and try again.
Unable to process the form. Check for errors and try again.