Caroticocavernous fistula
Updates to Study Attributes
Updates to Study Attributes
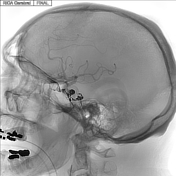
Supply from the right meningohypophyseal trunk to the right caroticocavernous fistula with retrograde opacification of the superior orbital vein.
Normal right external carotid artery branches without supply to the caroticocavernous fistula.
Opacification of right cavernous sinus noted, with likely previously partially thrombosed right inferior petrosal sinus and portions of the cavernous sinus. Venous microcatheter injections into the cavernous sinus confirm the caroticocavernous fistula anatomy visualized by right internal carotid artery injections, with eventual microcatheter position wedged into venous side of caroticocavernous fistula. Final images show Onyx cast in an appropriate position within cavernous sinus where the caroticocavernous fistula existed prior to embolization.
Right carotidICA angiogram after transvenous embolization with Onyx-18 demonstrates no opacification of the cavernous sinus.
CONCLUSION: Right caroticocavernous fistula supplied by the right meningohypophyseal trunk (Barrow type B); successfully embolized transvenously with Onyx-18.
Image DSA (angiography) (Internal carotid artery) ( update )
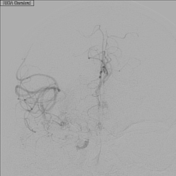
Image DSA (angiography) (Internal carotid artery) ( update )

Image DSA (angiography) (Internal carotid artery) ( update )
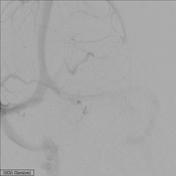
Image DSA (angiography) (External carotid artery) ( update )

Image DSA (angiography) (Right Inferior Petrosal Sinus) ( update )
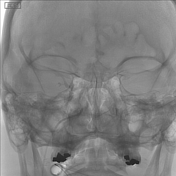
Image DSA (angiography) (Right Inferior Petrosal Sinus) ( update )
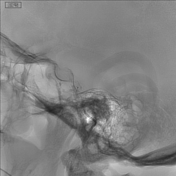
Image DSA (angiography) (Internal carotid artery) ( update )

Image DSA (angiography) (Internal carotid artery) ( update )
Updates to Case Attributes
55-year-old male with rapidly progressive right eye proptosis, chemosis, visual loss and orbital compartment syndrome due to a spontaneous Barrow type B indirect caroticocavernous fistula (shunt between meningohypophyseal trunk, an intracavernous branch of the internal carotid artery, and cavernous sinus). The patient initially was treated with antibiotics and steroids with no response. CTA and MRI findings suggested a caroticocavernous fistula. The patient underwent emergent lateral canthotomy with cantholysis and subsequent transvenous embolization of the caroticocavernous fistula Onyx-18 with symptomatic relief and residual blepharoptosis 9 months after treatment. The patient is planned for 9 mm right internal levator advancement for the treatment of blepharoptosis in the future.
-<p>55-year-old male with rapidly progressive right eye proptosis, chemosis, visual loss and orbital compartment syndrome due to a spontaneous <a href="/articles/barrow-classification-of-caroticocavernous-fistulae">Barrow type B</a> indirect <a href="/articles/caroticocavernous-fistula-1">caroticocavernous</a><a href="/articles/caroticocavernous-fistula-1"> fistula</a> (shunt between meningohypophyseal trunk, an intracavernous branch of the <a href="/articles/internal-carotid-artery-1">internal carotid artery</a>, and <a href="/articles/cavernous-sinus">cavernous sinus</a>). The patient initially was treated with antibiotics and steroids with no response. CTA and MRI findings suggested caroticocavernous fistula. The patient underwent emergent lateral canthotomy with cantholysis and subsequent transvenous embolization of the caroticocavernous fistula Onyx-18 with symptomatic relief and residual blepharoptosis 9 months after treatment. The patient is planned for 9 mm right internal levator advancement for the treatment of blepharoptosis in the future.</p>- +<p>55-year-old male with rapidly progressive right eye proptosis, chemosis, visual loss and orbital compartment syndrome due to a spontaneous <a href="/articles/barrow-classification-of-caroticocavernous-fistulae">Barrow type B</a> indirect <a href="/articles/caroticocavernous-fistula-1">caroticocavernous</a><a href="/articles/caroticocavernous-fistula-1"> fistula</a> (shunt between meningohypophyseal trunk, an intracavernous branch of the <a href="/articles/internal-carotid-artery-1">internal carotid artery</a>, and <a href="/articles/cavernous-sinus">cavernous sinus</a>). The patient initially was treated with antibiotics and steroids with no response. CTA and MRI findings suggested a caroticocavernous fistula. The patient underwent emergent lateral canthotomy with cantholysis and subsequent transvenous embolization of the caroticocavernous fistula Onyx-18 with symptomatic relief and residual blepharoptosis 9 months after treatment. The patient is planned for 9 mm right internal levator advancement for the treatment of blepharoptosis in the future.</p>
References changed:
- Korkmazer B, Kocak B, Tureci E, Islak C, Kocer N, Kizilkilic O. Endovascular Treatment of Carotid Cavernous Sinus Fistula: A Systematic Review. World J Radiol. 2013;5(4):143-55. <a href="https://doi.org/10.4329/wjr.v5.i4.143">doi:10.4329/wjr.v5.i4.143</a> - <a href="https://www.ncbi.nlm.nih.gov/pubmed/23671750">Pubmed</a>
- Chi C, Nguyen D, Duc V, Chau H, Son V. Direct Traumatic Carotid Cavernous Fistula: Angiographic Classification and Treatment Strategies. Study of 172 Cases. Interv Neuroradiol. 2014;20(4):461-75. <a href="https://doi.org/10.15274/INR-2014-10020">doi:10.15274/INR-2014-10020</a> - <a href="https://www.ncbi.nlm.nih.gov/pubmed/25207910">Pubmed</a>
- Lv X, Jiang C, Zhang J, Li Y, Wu Z. Complications Related to Percutaneous Transarterial Embolization of Intracranial Dural Arteriovenous Fistulas in 40 Patients. AJNR Am J Neuroradiol. 2009;30(3):462-8. <a href="https://doi.org/10.3174/ajnr.A1419">doi:10.3174/ajnr.A1419</a> - <a href="https://www.ncbi.nlm.nih.gov/pubmed/19131416">Pubmed</a>
- Lima V, Burt B, Leibovitch I, Prabhakaran V, Goldberg R, Selva D. Orbital Compartment Syndrome: The Ophthalmic Surgical Emergency. Surv Ophthalmol. 2009;54(4):441-9. <a href="https://doi.org/10.1016/j.survophthal.2009.04.005">doi:10.1016/j.survophthal.2009.04.005</a> - <a href="https://www.ncbi.nlm.nih.gov/pubmed/19539832">Pubmed</a>
- Annesley-Williams D, Goddard A, Brennan R, Gholkar A. Endovascular Approach to Treatment of Indirect Carotico-Cavernous Fistulae. Br J Neurosurg. 2001;15(3):228-33. <a href="https://doi.org/10.1080/02688690120057646">doi:10.1080/02688690120057646</a> - <a href="https://www.ncbi.nlm.nih.gov/pubmed/11478057">Pubmed</a>
- Korkmazer B, Kocak B, Tureci E et-al. Endovascular treatment of carotid cavernous sinus fistula: A systematic review. World J Radiol. 2013;5 (4): 143-55. <a href="http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3647206">Free text at pubmed</a> - <a href="http://www.ncbi.nlm.nih.gov/pubmed/23671750">Pubmed citation</a><span class="auto"></span>
- Chi CT, Nguyen D, Duc VT et-al. Direct traumatic carotid cavernous fistula: angiographic classification and treatment strategies. Study of 172 cases. Interv Neuroradiol. 2015;20 (4): 461-75. <a href="http://www.ncbi.nlm.nih.gov/pmc/articles/PMC4187443">Free text at pubmed</a> - <a href="http://www.ncbi.nlm.nih.gov/pubmed/25207910">Pubmed citation</a><span class="auto"></span>
- Lv X, Jiang C, Zhang J et-al. Complications related to percutaneous transarterial embolization of intracranial dural arteriovenous fistulas in 40 patients. AJNR Am J Neuroradiol. 2009;30 (3): 462-8. <a href="http://dx.doi.org/10.3174/ajnr.A1419">doi:10.3174/ajnr.A1419</a> - <a href="http://www.ncbi.nlm.nih.gov/pubmed/19131416">Pubmed citation</a><span class="auto"></span>
- Lima V, Burt B, Leibovitch I et-al. Orbital compartment syndrome: the ophthalmic surgical emergency. Surv Ophthalmol. 2009;54 (4): 441-9. <a href="http://dx.doi.org/10.1016/j.survophthal.2009.04.005">doi:10.1016/j.survophthal.2009.04.005</a> - <a href="http://www.ncbi.nlm.nih.gov/pubmed/19539832">Pubmed citation</a><span class="auto"></span>
- Annesley-Williams DJ, Goddard AJ, Brennan RP et-al. Endovascular approach to treatment of indirect carotico-cavernous fistulae. Br J Neurosurg. 2001;15 (3): 228-33. <a href="http://www.ncbi.nlm.nih.gov/pubmed/11478057">Pubmed citation</a><span class="auto"></span>







 Unable to process the form. Check for errors and try again.
Unable to process the form. Check for errors and try again.